Young Breast Cancer: A Changing Landscape in Early Adulthood
Today’s approach to breast cancer care is evolving rapidly. In the past, many envisioned the typical breast cancer patient as a middle-aged or older woman with an established life and grown children. However, a growing number of young adults—women in their 20s, 30s, and early 40s—are now facing a breast cancer diagnosis. This shift in demographics has brought to light several tricky parts and tangled issues that require specialized care. The Young Breast Cancer Program at Baptist Health Miami Cancer Institute is one such initiative that is working to address these subtle parts with speed, efficiency, and compassion.
This opinion piece explores how modern healthcare is adapting to the rising incidence of breast cancer in younger patients and what it means for the future of treatment. In doing so, we highlight how coordinated care, early detection, and tailored support play a super important role in addressing the unique needs of this population.
Addressing the Unique Needs of Younger Patients
The surge in breast cancer diagnoses among young women is not just a statistical anomaly—it is a call to action. Younger patients often present with more aggressive diseases that require immediate attention. Many of these women discover a lump or irregularity long after the ideal window for early detection has passed, making the cancer more advanced by the time of diagnosis. This creates a series of confusing bits and complicated pieces for both the patient and their healthcare providers.
For these reasons, specialized programs like the Young Breast Cancer Program have been designed to get patients to the right specialists as quickly as possible. This kind of coordinated care not only aims to address the cancer directly but also to manage the nerve-racking challenges of fertility preservation and the potential interruption of major life milestones such as completing education, establishing a career, or starting a family.
The Surprise of a Younger Onset
One of the most striking features of the current breast cancer landscape is the increasing number of women diagnosed before the age of 45. According to statistics from the American Cancer Society, about 10 percent of all new breast cancer diagnoses occur in this age group. At Miami Cancer Institute, this figure climbs to roughly 13 percent. These numbers indicate that breast cancer is no longer solely an ailment of older age, and they underscore the importance of early intervention and patient education.
Below is a table summarizing the differences between typical older onset and younger onset breast cancer cases in terms of detection and aggressiveness:
| Aspect | Older Onset | Younger Onset |
|---|---|---|
| Detection Method | Regular screening (mammograms) | Self-discovery; diagnostic imaging post-symptom detection |
| Cancer Aggressiveness | Often slower growing | Potentially more aggressive |
| Patient Life Stage | Established family, career, and social networks | College, early career, starting families, and building social dynamics |
This table illustrates the subtle differences that matter when considering treatment strategies, highlighting the nerve-wracking realities many young women face. It also shows the critical importance of tailored screening and early intervention programs.
Streamlined Care Coordination: A Critical Approach
The Young Breast Cancer Program is built on the idea that timely and coordinated care can make a significant difference for young patients. This approach reduces the overwhelming stress of having to coordinate multiple appointments, referrals, and tests simultaneously—all at a time when decisions need to be made quickly.
Immediate Comprehensive Evaluations
When a patient under the age of 45 is diagnosed with breast cancer, time is of the essence. Intake nurses and nurse navigators are immediately alerted to ensure that the patient is fast-tracked into the system. This means that rather than worrying about making endless phone calls or figuring out complex appointment schedules, the patient can focus on preparing mentally and emotionally for the steps ahead.
Such rapid coordination minimizes the tangled issues of starting chemotherapy quickly while also considering other equally important referrals, such as those for onco-fertility, genetic counseling, and reconstructive surgeries. The program’s design ensures that every critical facet of the cancer journey is managed simultaneously, reducing the stressed missteps that might otherwise occur when a patient is left to make her own way for every part of the process.
Benefits of a Coordinated Approach
A few bullet points highlight how streamlined care benefits younger breast cancer patients:
- The patient receives a complete workup in a short period, minimizing delays.
- Multidisciplinary referral systems ensure that each aspect—ranging from fertility preservation to genetic testing—is seamlessly integrated.
- Patients experience less pressure and reduced stress, allowing them to take a closer look into the treatment ahead with a calm mindset.
- Early enrollment in support and educational programs can help ease the emotional burden during treatment decisions.
For many young women, these steps offer hope and reassurance at a time when every minute counts. By minimizing the confusing bits in the process, the program empowers patients to care for both their physical and emotional well-being throughout treatment.
Compassionate and Coordinated Care: The Keystone of Treatment
One of the most striking aspects of the Young Breast Cancer Program is its emphasis on compassion. Managing a new diagnosis is not only physically taxing, but it also involves a nerve-racking amount of emotional stress. For many patients, the reality of a cancer diagnosis comes with a myriad of daunting life questions and sudden twists and turns that affect their future family planning and career goals.
In this regard, having a healthcare team that is both empathetic and efficient is super important. The program is staffed by knowledgeable experts, including Dr. Starr Mautner, Dr. Jane Mendez, and Dr. Reshma Mahtani, each of whom brings a unique perspective to the table. Their roles are not just to treat the cancer but also to guide their patients through the tangled maze of associated challenges—be it preserving fertility, managing immediate care needs, or planning post-treatment recovery.
Multidisciplinary Teams: Finding Your Path to Recovery
Effective breast cancer care requires integrating advice and treatment from various experts. The following list provides an overview of the types of specialists involved and what they address:
- Breast Surgical Oncologists: These doctors assess the tumor and perform necessary surgical interventions. Their work often involves discussing reconstructive options and facing the demanding pieces of treatment planning.
- Medical Oncologists: Responsible for overall cancer management, they strategize on chemotherapy and other drug therapies while anticipating potential side effects.
- Fertility Specialists: For younger women desiring future pregnancies, these experts discuss options such as egg or embryo storage, catering to the unique twists and turns of reproductive planning.
- Genetic Counselors: With genetics playing a crucial role in some cases, counselors help patients understand the risks that might be inherited.
- Plastic and Reconstructive Surgeons: These professionals assist with cosmetic and reconstructive decisions, critical after surgery to ensure the patient’s quality of life is maintained.
This integrated approach ensures that the little details of a patient’s overall well-being are addressed with precision and empathy. Instead of facing these issues in isolation, patients benefit from the collective knowledge and care of professionals who work together to manage every twist and turn.
Personal Stories: The Human Side of Young Breast Cancer
An essential element of any healthcare transformation is the human experience. Many young women who have undergone treatment become active in their communities by leading support groups, spearheading fundraising events, or starting awareness campaigns on social media. These personal victories not only provide hope to others in similar situations but also underscore the importance of compassionate care.
For instance, Dr. Mautner, who is both a young breast surgeon and a mother, often shares how her personal experience deepens her understanding of what her patients are going through. Observing a patient regain her ability to live a fulfilling life—whether that means pursuing a career, having children, or engaging in community activities—serves as a powerful motivator for healthcare providers.
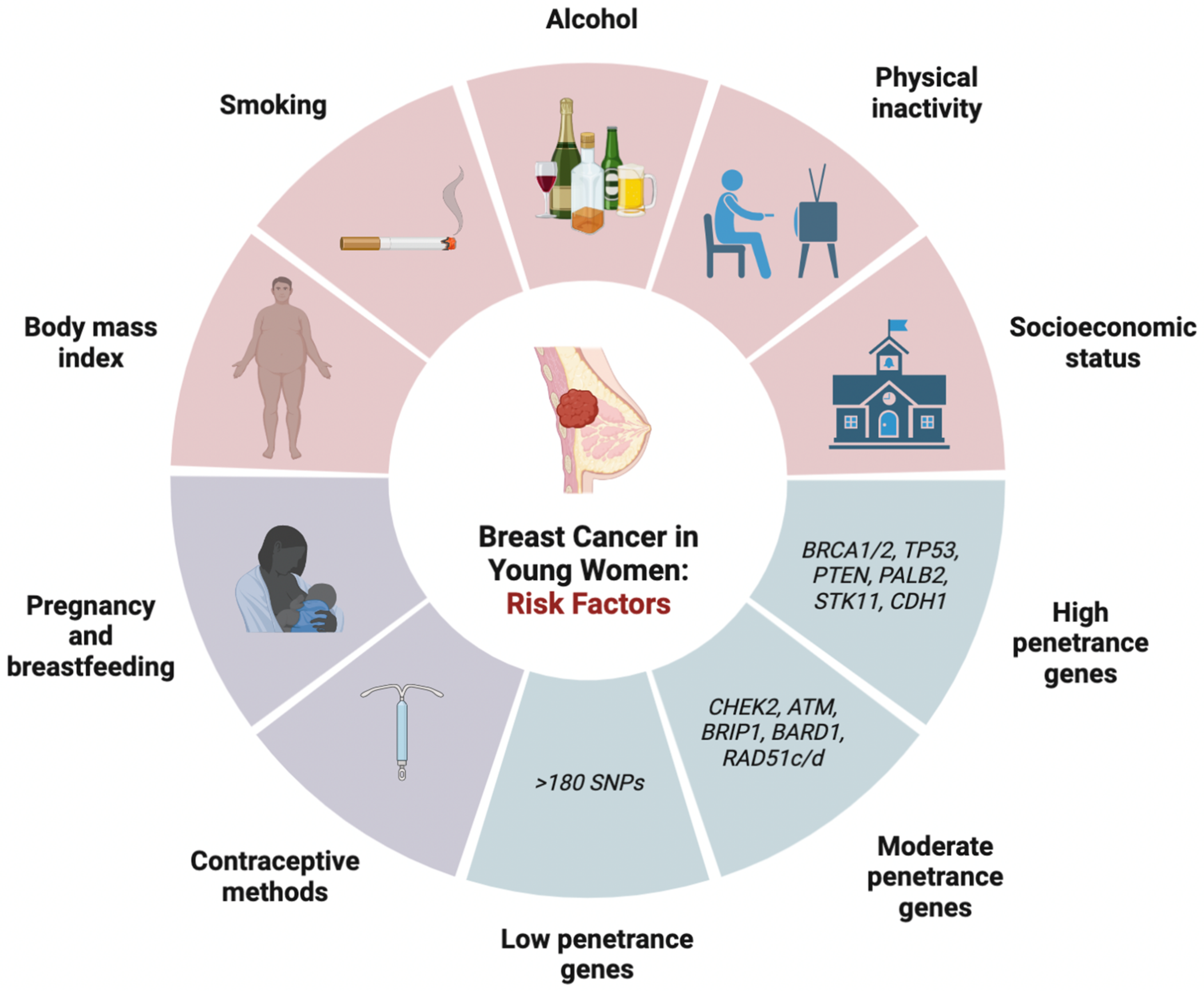
Understanding Breast Cancer Risk in Early Adulthood
Risk factors for breast cancer in younger women are both varied and challenging to untangle. In addition to genetic predispositions, factors such as lifestyle, diet, and environmental exposures also play a role in determining risk levels. Given the many confusing bits and nerve-wracking questions that come with a positive diagnosis, early conversations between patients and their doctors can help set a clear path forward.
Primary care physicians and OB/GYNs are super important when it comes to identifying individual risk factors and tailoring early screening recommendations. The idea is not only to treat cancer when it appears but also to adopt a proactive strategy to prevent it from taking root. Women with a family history of cancer, known genetic mutations, or other red flags should start these discussions well before their 30th birthday.
Key Lifestyle Considerations and Preventive Measures
While some risk factors, like family history, are unchangeable, many aspects of a person’s lifestyle can be adjusted to potentially lower the risk of developing breast cancer. Health educators and experts often emphasize the need for a healthy lifestyle as a means to steer through these tangled issues.
- Nutrition: Maintaining a balanced diet rich in fruits, vegetables, and lean proteins can reduce cancer risk. Anti-inflammatory foods and antioxidants have been shown to help balance out oxidative stress in the body.
- Physical Activity: Regular exercise is not only key for overall health but also plays a role in managing weight and reducing breast cancer risk. Even activities like walking or yoga can help get the blood flowing and relieve stress.
- Alcohol Consumption: Limiting alcohol is recommended as excessive intake has been linked to an increased risk of breast cancer. Moderation is key to avoiding additional risk factors.
- Weight Management: Keeping a healthy weight can lessen the likelihood of hormone-related cancers, including breast cancer. A consistent approach to diet and fitness can make all the difference.
By focusing on these areas, women can actively figure a path to lower their overall risk. Every appointment, every lifestyle modification, and every educational conversation serve as reminders of the importance of prevention, even in the absence of a definitive diagnosis.
The Role of Genetics and Environmental Factors
Healthcare experts agree that a combination of genetic, environmental, and lifestyle factors contributes to the increased incidence of breast cancer among younger women. While the exact reasons remain on edge and full of problems, factors such as exposure to certain chemicals, stress levels, and even dietary trends can play a role.
For instance, the consumption of processed foods and high levels of alcohol are often mentioned as contributors. At the same time, environmental pollutants might add to the overall risk profile. As healthcare providers continue to get into research and analyze clinical data, a more complete picture of these hidden complexities is gradually emerging.
Enhancing Research to Improve Future Outcomes
One of the most promising aspects of the Young Breast Cancer Program is its commitment to research. By creating a comprehensive database that captures both clinical and genomic information from young patients, physicians hope to answer key research questions. This data-driven approach may one day reveal why breast cancer rates are climbing among young women and how outcomes can be improved with targeted interventions.
A multidisciplinary research initiative like this not only focuses on immediate patient care but also builds a foundation for future breakthroughs. Some areas of research that are being closely monitored include:
- Patterns in Disease Aggressiveness: By studying the specific ways in which breast cancer manifests in young women, researchers hope to identify trends that can lead to more personalized treatment methods.
- Genomic Profiling: The integration of genetic data supports the identification of markers that could indicate an increased risk, leading to earlier interventions.
- Treatment Response Analysis: Monitoring how younger patients react to various therapies over time may offer insights into optimizing treatment sequences and combinations.
- Impact of Lifestyle Factors: Long-term studies that correlate dietary and environmental factors with breast cancer outcomes are proving essential in understanding this dynamic risk profile.
These research efforts are essential for moving toward more individualized and effective treatment strategies. Over time, they may help healthcare providers better manage the nerve-wracking timeline of treatment decisions and reduce the overall burden on young patients.
Practical Strategies for Young Women Facing Breast Cancer
Beyond the clinical and research breakthroughs, there are practical strategies that young women can adopt when confronted with a breast cancer diagnosis. These tips are designed to help manage the immediate challenges that come with the diagnosis, as well as the long-term implications for life, career, and family planning.
Coping with a Diagnosis and the Immediate Steps Forward
Receiving a breast cancer diagnosis at any age is overwhelming. For young women, the situation is especially challenging because they must quickly figure a path through treatment choices without delaying the start of therapy. Here are some practical steps to consider:
- Open Communication with Your Healthcare Team: Ask as many questions as needed to fully understand the treatment options. Whether it’s discussions on chemotherapy, radiation, or surgery, clarity is key.
- Engage with Support Services: Many centers offer counseling, support groups, and patient navigators. Utilizing these services can help ease the intimidating aspects of decision-making.
- Discuss Fertility Preservation Options Early: If planning to have children in the future, talk to a fertility specialist as soon as possible. This is a critical conversation that should occur without delay.
- Stay Informed: Educate yourself about both the risks and the treatment protocols. Reliable information can reduce the overwhelming feelings of facing this nerve-wracking diagnosis.
Taking these steps not only facilitates a smoother treatment process but also empowers patients to take charge of their own healthcare. It is important to remember that while the journey might be challenging, you are not alone—your healthcare team is there to help you sort through the many tangled issues.
Building a Support Network: Family, Friends, and Community Resources
Beyond clinical care, social support plays a super important role in recovery. Family members, friends, and community organizations provide the emotional boosts needed during treatment. Here are several ways a young breast cancer patient might build a strong support network:
- Join a Patient Support Group: Community groups and online forums can be invaluable for sharing experiences and practical advice.
- Engage in Lifestyle Communities: Whether it’s fitness groups, nutritional classes, or mindfulness workshops, these communities help restore a sense of normalcy and encourage well-being.
- Work with a Patient Navigator: Many health programs have dedicated professionals to help manage appointments, referrals, and follow-up care, lightening the load considerably.
- Consider Mental Health Counseling: Professional counseling or therapy can help manage the significant stress and slight differences in emotional trauma that often come with a cancer diagnosis.
Harnessing the power of a supportive community can turn an intimidating journey into one where hope and resilience shine through. The actions of community members, combined with professional guidance, help young patients manage the stressful aspects of treatment.
The Future of Breast Cancer Care for Young Patients
As breast cancer continues to affect an increasing number of younger women, the healthcare community is working hard to respond with innovative care models and integrated support programs. The future of breast cancer care is likely to be shaped by both patient-centric approaches and advances in medical technology, all built on a foundation of streamlined care and ongoing research.
Programs like the Young Breast Cancer Program at Baptist Health Miami Cancer Institute demonstrate that by quickly integrating multidisciplinary care, eliminating the confusing bits of treatment coordination, and addressing the nerve-racking challenges head-on, patients can have better outcomes. There is hope that, with ongoing research and improved care models, the trends seen today will ultimately lead to a decrease in advanced cases discovered in young women.
Innovative Technologies and Their Role in Future Treatment
Technological advancements are also playing a significant role in shaping the future of breast cancer care. Innovations include the use of advanced imaging, precision medicine, and targeted radiation therapies. These tools not only help detect tumors earlier but also allow for more individualized treatment plans that take into account the fine points of each patient’s condition.
For example, advanced MRI-guided radiation therapy and emerging robotic surgery techniques are being experimented with to determine how best to minimize side effects while maximizing treatment effectiveness. When employed as part of a coordinated and compassionate care strategy, these technologies provide optimism for both young patients and the broader medical community.
Empowering Young Patients Through Education and Advocacy
A continued emphasis on learning and advocacy is essential. As more young women are diagnosed with breast cancer, education becomes a powerful tool to demystify the disease and its treatment options. The sharing of personal stories, support group experiences, and professional insights helps to create an environment where patients can feel empowered.
It is equally critical that healthcare providers work with public health agencies to spread awareness about early screening and the importance of understanding one’s personal risk factors. Educational campaigns that delve into the subtle details of breast cancer symptoms and treatment plans help demystify the process and guide patients safely through their journeys.
Concluding Thoughts
In conclusion, the evolving landscape of breast cancer in young women calls for a renewed emphasis on compassion, swift coordinated care, and proactive research. The Young Breast Cancer Program serves as a model for what can be achieved when the healthcare community steps up to address the unique needs of a vulnerable population. With rapid diagnosis, integrated support, and a commitment to ongoing research, young patients are given the best possible chance to face treatment head-on.
While there remain many tricky parts and tangled issues along the way, programs like these are helping to transform what once was an overwhelming and off-putting diagnosis into a journey of hope, support, and recovery. By embracing an approach that combines science, technology, and human compassion, we are laying the groundwork for a future where every young woman has access to the must-have services she needs, both medically and emotionally.
Ultimately, every conversation, every research breakthrough, and every improvement in care coordination is a step toward ending the narrative of fear that has long accompanied a breast cancer diagnosis. As we continue to work through the many little details in this journey, we must remember that every young patient deserves a chance not just to survive, but to thrive—to build careers, families, and lives enriched by the supportive embrace of a truly caring health system.
The path forward is clear: early detection, comprehensive care, and compassionate support must become the hallmarks of breast cancer treatment for young women. Together, healthcare providers, researchers, and communities can turn the tide against a disease that has, for too long, carried the heavy burden of uncertainty and hardship. Through perseverance and innovation, we are finding our way toward a future where breast cancer care is not only sophisticated but also deeply human.
Originally Post From https://baptisthealth.net/baptist-health-news/young-breast-cancer-program-better-care-coordination-for-patients
Read more about this topic at
Compassionate Coordinated Care – to help save lives from …
Operationalizing Compassionate Connected Care