Introduction: Understanding DVT Risk After Traumatic Brain Injury
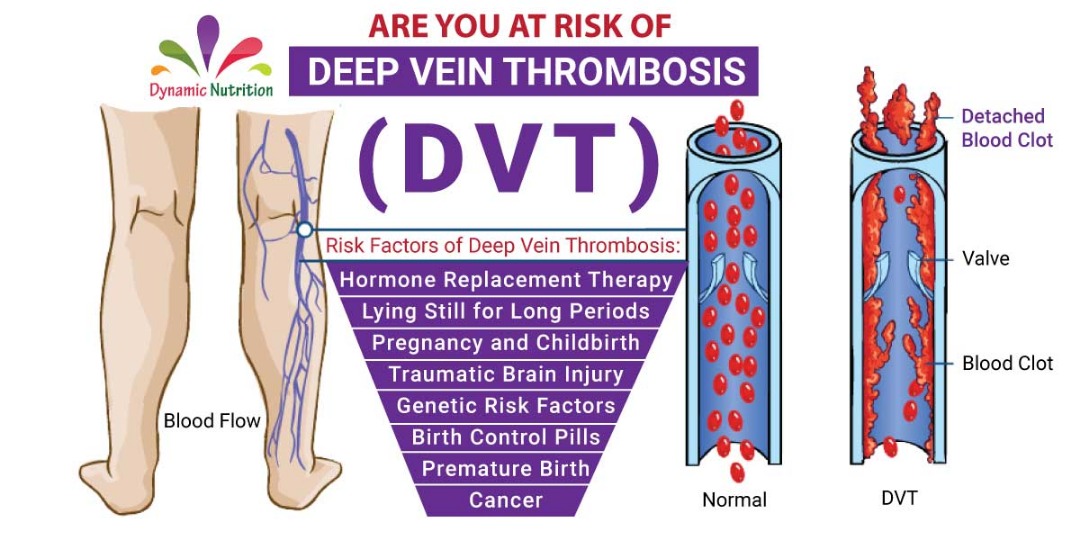
Deep vein thrombosis (DVT) remains a serious health issue for patients recovering from traumatic brain injury (TBI). In recent years, clinicians have been working through the tangled issues of early DVT identification to improve outcomes in TBI cases. A recent study utilized a nomogram model that combines several risk factors to predict the likelihood of postoperative DVT. As an opinion editorial, this article explores the clinical promise of such models, discusses their benefits and limitations, and offers insight into how healthcare professionals can figure a path through the tricky parts of TBI management.
At its heart, the research identified eight key risk factors, including age, BMI, smoking history, fluid intake and output balance, interval between surgery and injury, and three important laboratory markers (D-dimer, fibrinogen, and prothrombin time). By integrating these elements into a visual, user-friendly nomogram, clinicians can more effectively predict DVT risk and plan early interventions. The purpose here is to reflect on this approach, compare it with traditional practices, and consider future directions for clinical integration.
Early Warning Signs: Essential Risk Factors in TBI Patients
One of the benefits of any predictive model is its ability to bring to light risk factors that might otherwise be lost among the confusing bits of clinical data. In the context of TBI, patients are already dealing with severe outcomes, and overlooking early signs of DVT can lead to additional complications that extend hospital stays and increase overall healthcare costs.
The research in question identified several key risk indicators. By breaking down each factor, we can appreciate how these seemingly small elements play a super important role in risk stratification.
Age, BMI, and Smoking: The Common Culprits
It is widely acknowledged that older age and an elevated BMI are connected with an increased chance of DVT. Over the years, clinicians have suspected that older patients or those who are overweight might face higher blood viscosity and sluggish blood flow. The study reinforces that these factors are indeed a concern among TBI patients. Moreover, a history of smoking further aggravates the situation.
Smoking not only contributes to vascular damage but also promotes the release of harmful vasoactive substances. As a result, smoking adds another layer of risk that can compound with age and obesity. Together, these factors present a scenario where the risk of clot formation is markedly elevated.
In summary, the bullet points below capture these risk factors:
- Advanced Age: Associated with slower metabolism and weakened vessel elasticity.
- High Body Mass Index (BMI): Leads to increased blood viscosity and potential clot formation.
- Smoking History: Damages vascular walls and enhances prothrombotic conditions.
Fluid Balance and Surgery Timing: The Tricky Parts
A less obvious but equally important consideration is the balance of fluid intake and output. A negative balance—where outflow exceeds inflow—can lead to dehydration. This state causes blood to become more concentrated, resulting in a higher risk for clotting. In TBI management, where fluid management is already a delicate task, the need to pay attention to these details cannot be overstated.
Furthermore, the interval between the injury and the operation is another key factor. When this interval exceeds six hours, the risk of DVT increases significantly. The longer waiting time might be associated with prolonged immobility and the gradual onset of a hypercoagulable state, where the blood finds it easier to clot.
The following table offers a concise view of these clinical factors:
| Risk Factor | Impact |
|---|---|
| Negative Fluid Balance | Increases blood viscosity and clot risk |
| Delayed Surgery (>6 hours) | Enhances prolonged immobility and a hypercoagulable state |
Laboratory Markers: D-dimer, Fibrinogen, and Prothrombin Time
In addition to clinical assessments, laboratory markers provide objective insight into the body’s coagulation status. Among these, D-dimer stands out as a critical gauge. Elevated D-dimer levels reflect active clot formation and breakdown—a sign that the body is responding to a thrombogenic stimulus. Fibrinogen levels, too, hold significance; elevated fibrinogen is often linked to an increased readiness for clot formation, while a reduced prothrombin time indicates that the blood may clot more quickly than normal.
Understanding these markers becomes easier when we list them as follows:
- D-dimer: High levels indicate active clotting and fibrinolysis.
- Fibrinogen (FIB): Elevated levels increase the likelihood of clot formation.
- Prothrombin Time (PT): Shorter PT can signal hypercoagulability.
By considering these clinical and laboratory factors together, the model provides a multi-dimensional view of DVT risk. Physicians can use such detailed insights to construct personalized treatment plans for TBI patients, aiming for early prevention and timely intervention.
The Nomogram Model: A Clear Guide for Clinicians
Nomograms are graphical tools that provide a visual representation of complex multivariate statistical models. The nomogram model discussed in the recent study has been designed to predict the risk of DVT in TBI patients by combining key patient variables. For many healthcare professionals, this tool is not only a prediction model but also a roadmap that helps steer through the risky territory of postoperative complications.
The model constructed from the study includes eight non-zero coefficient variables: age, BMI, smoking history, fluid balance, time between surgery and injury, and preoperative measurements of D-dimer, fibrinogen, and prothrombin time. Clinicians assign points to each risk factor, sum them up, and arrive at a probability of developing DVT. The beauty of the nomogram lies in its straightforward approach, which makes it super important for translating clinical data into actionable insights.
Benefits of the Nomogram in Postoperative Care
The advantages of integrating a nomogram into clinical practice are numerous. Here are some of the key benefits:
- Ease of Use: The tool offers a simple calculation method that does not require extra software or complicated statistical knowledge.
- Visual Representation: By using a clear chart format, clinicians can quickly grasp the risk level, which aids in making timely decisions.
- Cost-Effective: Because the model leverages commonly available clinical and laboratory data, it does not add financial or procedural burdens to patient care.
- Personalized Risk Assessment: It enables doctors to provide a tailored evaluation for each patient, allowing for early intervention and targeted management strategies.
- Integration Potential: The simplicity of the nomogram makes it a candidate for incorporation into existing electronic health record systems, where real-time alerts can be generated.
In cases where time is of the essence, having a tool that helps clinicians get into the nitty-gritty without being overwhelmed by the fine points is a major advantage. It ensures that early, proactive care measures are taken, potentially reducing complications and improving patient outcomes.
Clinical Decision Making: From Data to Action
While statistical models can sometimes seem intimidating due to their small distinctions and hidden complexities, what matters most is how they translate into everyday clinical practice. The nomogram provides clinicians with a clear forecast regarding early DVT risk, which in turn supports swift, evidence-based decision making. When a patient is identified as being at high-risk, measures such as early ultrasound screening, appropriate prophylactic anticoagulation, and close monitoring of fluid balance can be initiated.
It is also important to highlight that clinical decision curve analysis has supported the model’s usefulness. In simple terms, decision curves have shown that when the chances of a DVT are high enough, intervention based on nomogram predictions offers a significant net benefit. By converting data into tangible advice, healthcare providers can confidently work through the twists and turns of TBI management.
Intervention Strategies and Preventive Measures
A proactive approach toward preventing DVT in TBI patients is critical. Based on the risk factors identified and the predictions provided by the nomogram, healthcare professionals can consider several intervention strategies:
- Early Ultrasonic Screening: Conducting lower limb ultrasounds as soon as possible—especially within the first three to seven days post-operation—helps in early detection.
- Fluid Management: Monitoring and correcting a negative fluid balance can reduce blood concentration and lower the risk of clot formation.
- Timely Prophylactic Anticoagulation: Implementing low molecular weight heparin or other safe anticoagulation protocols based on an individual’s risk assessment can be decisive.
- Lifestyle Modifications: Advising patients to reduce smoking and encouraging early mobilization where possible can have a lasting impact on recovery.
These measures are not only practical but also grounded in everyday clinical experience. When healthcare providers have a tool that helps them pinpoint which patients are most at risk, they can move quickly to mitigate complications.
Limitations, Challenges, and the Way Forward in Risk Modeling
Despite the promising nature of the nomogram model, several limitations remain that warrant discussion. No single model can capture every detail of a complex clinical scenario, and there are always tricky parts that need careful consideration.
A primary concern is the study’s reliance on retrospective data. While the model shows high prediction accuracy (with an AUC reaching around 0.83 in the training set and 0.82 in the validation set), the retrospective design and relatively small sample size may introduce bias and issues related to overfitting. These challenges remind us that even the best predictive tools have hidden complexities that need addressing with further research.
Sample Size and Overfitting Concerns
Even though the study involved patients from two different centers, the total number of cases was limited. A smaller sample size can create a scenario where the model appears more accurate than it might be when subjected to a broader and more diverse patient population. The risk of overfitting—where the model learns the small details of a particular dataset that do not translate well into general practice—is a genuine concern.
Some of the issues stemming from these concerns might include:
- Potential bias due to retrospective data collection.
- The risk that the model may not perform as well in different clinical settings.
- A need for more extensive, prospective data to solidify the findings.
Need for Prospective Studies and Time-to-Event Data
Another area where the current model could be improved is in capturing the exact timing of DVT onset. Presently, the nomogram does not incorporate time-to-event data. This is a significant limitation, as knowing when a patient is most likely to develop DVT could help in tailoring the timing of preventive interventions.
Future research should consider the following enhancements:
- Conducting large-scale, prospective studies to confirm and expand on the current findings.
- Integrating time-to-event analysis to refine the risk predictions further.
- Externally validating the model in different healthcare settings to ensure broader applicability.
- Using advanced statistical approaches to mitigate any residual risk of overfit and to incorporate additional clinical variables that might be relevant.
While these challenges may seem intimidating, they are not insurmountable. With continued research efforts and a willingness to integrate clinical data with modern analytical tools, the healthcare community can work through these problematic bits to enhance patient safety.
Opinion: Integrating Predictive Models in Everyday Clinical Practice
Predictive models like the nomogram discussed here hold significant promise for improving clinical outcomes in TBI patients. In everyday practice, physicians are inundated with a vast amount of information, and time is often not on their side. A model that quickly aggregates key variables and presents an easy-to-understand risk score can be a game-changer.
In my view, the strengths of such methods lie in their simplicity and their direct clinical relevance. When the model provides a visual aid that clearly shows the probability of developing a dangerous condition like DVT, doctors can respond more swiftly. The integration of routine laboratory data means that no extra tests are needed, saving both time and resources. In a busy hospital setting, that is a major plus.
The integration of these tools into electronic health record systems could be a realistic goal in the near future. For example, a patient admitted with TBI can have their routine labs automatically processed, and the system could trigger an alert if the predicted risk of DVT is high. This kind of proactive warning might lead to timely preventive measures, such as early anticoagulation or mobilization protocols.
Real-World Challenges Versus Research Promises
Although the model shows strong potential, translating research findings into real-world practice is not always straightforward. The model’s impressive performance in controlled studies may be met with mixed reviews when integrated into the everyday clinical environment, where patient differences can be more pronounced and treatment regimens more complex.
Real-world application means healthcare professionals have to figure a path through several additional challenges:
- Training and Adoption: Clinicians must be adequately trained to use the nomogram so that the small distinctions it provides are interpreted correctly. This is especially important given that the tool is based on data that may evolve over time.
- Integration with Existing Workflows: For the nomogram to be truly useful, it must be seamlessly integrated into the existing electronic medical record systems. Otherwise, extra steps in the workflow could deter its use.
- Continuous Validation: As new data emerge, it is critical to keep improving the model. Continuous external validation will help ensure that the model remains robust and relevant across different patient populations.
Even with these real-world challenges, it is clear that tools like the nomogram can assist in addressing the overwhelming issues that many clinical practitioners face when making rapid decisions. In this dynamic field, combining clinical judgment with data-driven insights remains the best strategy for managing patient care effectively.
Concluding Thoughts: Balancing Model Data and Clinical Judgment
Ultimately, the integration of predictive models into clinical practice is an exciting step forward in modern medicine. The nomogram model for predicting DVT risk after TBI offers a clear and approachable method for early risk assessment. By combining routine clinical and laboratory data, it provides a window into the hidden complexities of postoperative care, allowing for tailored interventions and improved outcomes.
However, it is important to remember that while such models are super important for guiding decision-making, they should not be seen as complete substitutes for clinical judgment. The human element in medicine—where a doctor’s experience, intuition, and the ability to adapt to subtle details—remains indispensable. A tool like the nomogram is best used as an adjunct: a resource that provides critical insights to support, rather than replace, the nuanced decision-making process of clinicians.
Key takeaways from this discussion include:
- Early Identification: Recognizing risk factors such as advanced age, high BMI, smoking history, fluid imbalance, delayed surgery, and abnormal lab markers is crucial for managing DVT risk in TBI patients.
- User-Friendly Tools: Predictive models and nomograms offer a straightforward, visual way to assess risk, which can be seamlessly integrated into everyday clinical practice.
- Proactive Clinical Management: With early risk predictions, interventions such as early ultrasound screenings, careful fluid management, and timely prophylactic treatments can be administered to mitigate risk.
- Continuous Improvement: The current model, while promising, needs further validation and refinement. Prospective studies with larger sample sizes and time-to-event analyses are crucial for ensuring its ongoing relevance.
- Balanced Decision Making: Ultimately, predictive models should complement a clinician’s expertise, providing an extra layer of data that supports but does not override direct patient care decisions.
As we move forward, the ongoing dialogue between research and practical implementation is essential. The collaboration between data scientists, clinicians, and hospital administrators will shape a future where predictive models are a natural part of medical decision-making. This collaborative approach holds the promise of reducing postoperative complications, shortening hospital stays, and ultimately saving lives.
While the twists and turns of integrating new technology into established clinical workflows can be a bit nerve-racking, the potential benefits justify these efforts. The model represents a step toward precision medicine where every patient receives care that is custom-tailored to their unique risk profile. By using resources like the nomogram, we not only boost the quality of care but also support healthcare providers in managing the challenging and often time-sensitive conditions that TBI patients face.
In conclusion, balancing the rich data provided by predictive models with the specialized judgment of clinicians everywhere can lead to better outcomes for patients prone to deep vein thrombosis. As we continue to work through the tricky parts of translating academic research into everyday practice, it is hoped that models like this one serve as an essential part of the future of patient care.
Embracing these technologies now may well pave the way for a more efficient, cost-effective, and patient-centered approach to healthcare—an endeavor that is surely in the best interests of both practitioners and the communities they serve.
Originally Post From https://www.nature.com/articles/s41598-025-15287-z
Read more about this topic at
A Nomogram Model to Predict Deep Vein Thrombosis Risk …
A prediction nomogram for deep venous thrombosis risk in …