Digging Into Traumatic Brain Injury and Blood–Brain Barrier Protection
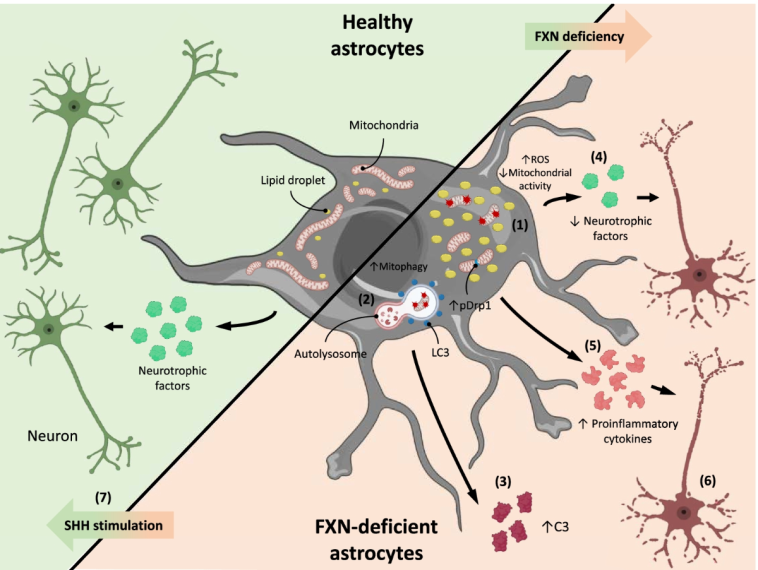
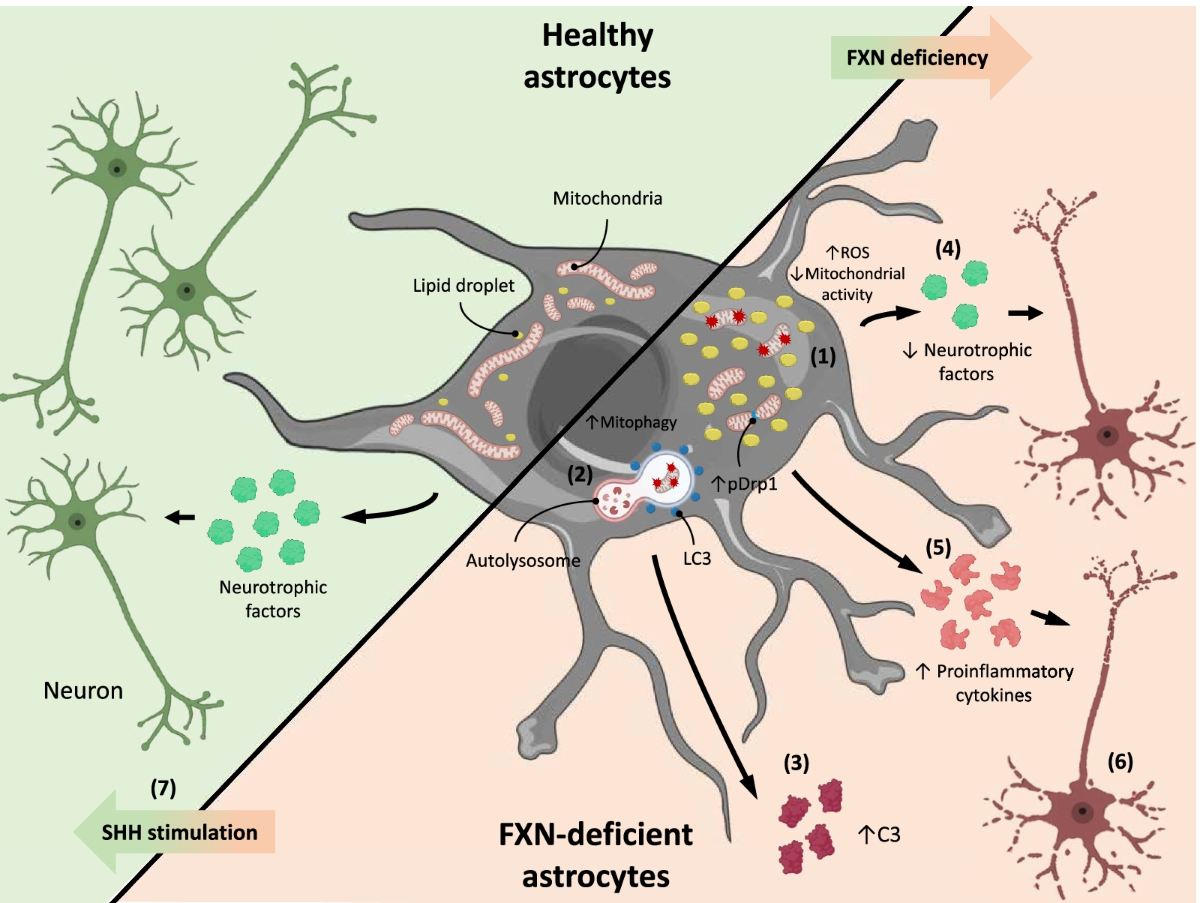
Traumatic brain injury (TBI) remains one of the most challenging brain conditions, full of problems that extend far beyond the initial shock. When the brain suffers an impact from accidents or falls, the tangled issues of blood–brain barrier disruption, brain edema, and neuroinflammation begin a chain reaction that can lead to long-lasting neurological dysfunction. Recent research has been shedding new light on this critical area, with an emphasis on how the sonic hedgehog (Shh) signaling pathway and its downstream mediator, smoothened (Smo), might offer key strategies to protect the brain’s integrity.
Many readers might not be familiar with the fine points of how the blood–brain barrier (BBB) operates in safeguarding the brain. Essentially, the BBB functions as a gatekeeper, ensuring that harmful substances in the bloodstream do not penetrate sensitive brain tissue. However, when TBI occurs, the BBB becomes leaky, leading to vasogenic edema—a build-up of water in the brain—as well as the infiltration of inflammatory cells. Such events trigger a chain reaction that makes the road to recovery a nerve-racking and intimidating journey for patients.
Understanding the Sonic Hedgehog Pathway in Brain Health
A growing body of literature has been exploring the hidden complexities of the Shh signaling pathway. This pathway is not only essential for brain development but also plays a pivotal role in repairing the damaged brain. One of the most interesting aspects of recent research is the observation that after TBI, there is an upsurge in the production of Shh along with its regulatory proteins, such as patched-1 (Ptch-1) and smoothened (Smo).
This research suggests that the brain’s own repair mechanisms kick in shortly after injury. The increase in Shh signals may encourage the production of proteins vital for repairing the BBB and reducing cerebral edema. However, the exact mechanisms for these effects are still full of tricky parts, and scientists continue to poke around to get into the fine shades that differentiate repair from further damage.
How Shh Protects the Blood–Brain Barrier
One key outcome of these studies is the realization that exogenous Shh—or Shh introduced from outside the body—appears to bolster the integrity of the BBB. In laboratory settings, administering recombinant Shh (rShh) alleviated the severity of vasogenic edema resulting from TBI. By increasing the expression of tight junction proteins (TJPs) such as claudin-5 and occludin, the treatment limited the escape of fluids into the brain tissue.
This process is vital because when you think about it, the BBB is like a wall with very fine gaps. Tight junction proteins act as the mortar holding together the bricks of this wall. When these proteins are reduced after an injury, the wall starts to crumble, letting inflammatory substances cause further damage. Restoring or even enhancing these proteins is a super important step in the healing process.
- Increased TJP expression strengthens the BBB.
- Improved barrier function helps prevent vasogenic edema.
- Reduced leakage also diminishes local neuroinflammation.
It’s the kind of approach that promises to redirect therapy from merely treating the symptoms to dealing with the nerve-racking twists and turns that happen right at the source of the injury.
Exploring the Roles of Astrocytes and Endothelial Cells
When discussing TBI and its aftermath, it is important to note that astrocytes and brain endothelial cells are two of the main players. Astrocytes, a type of glial cell, are often the first to respond to injury. They help in recycling neurotransmitters, maintaining ion balance, and, crucially, producing Shh. Recent in vitro experiments have shown that traumatic injury models can stimulate astrocytes to upregulate Shh, suggesting that these cells might be taking the lead in rallying the brain’s defenses.
On the other hand, brain endothelial cells, which make up the lining of the BBB, also experience significant changes post-injury. The tricky parts of their response include not only a decrease in TJPs but also subtle differences in the expression of Smo and Ptch-1. These cells are very sensitive to tissue damage and are integral to the repair process once activated by signals from astrocytes.
Charting the Cellular Response
Understanding the interactions between astrocytes and endothelial cells is key to sorting out the intertwined relationship between inflammation and repair post-TBI. Researchers have observed that when Shh levels rise, both astrocytes and endothelial cells increase the expression of proteins that help restore the BBB and mitigate inflammatory signals.
| Cell Type | Key Role | Response After TBI |
|---|---|---|
| Astrocytes | Primarily produce Shh | Increase Shh production to initiate repair |
| Endothelial Cells | Form the BBB | Upregulate tight junction proteins and Smo signaling components |
This table summarizes some of the little details involved in the cellular interplay after a brain injury. While the research is still ongoing, it is clear that the dialogue between these cell types forms the backbone of how the brain manages its recovery.
Tackling Vasogenic Edema and Neuroinflammation With Smo Agonists
One of the nerve-racking challenges after TBI is the onset of vasogenic edema—a condition where water swells brain tissue due to BBB leakage. Standard therapies have struggled with the confusing bits of edema reduction because of the off-putting side effects often seen in traditional anti-inflammatory drugs. Recent studies, however, highlight the potential of Smo agonists as a promising therapeutic strategy.
You might be wondering: what exactly is a Smo agonist? In simple terms, these are compounds that activate the smoothened receptor—a crucial component of the Shh signaling pathway. Among these, small-molecule compounds such as SAG (Smoothened Agonist) have received significant attention. What makes SAG particularly notable is its ability to cross the BBB following intravenous administration, potentially offering a more practical treatment for TBI.
How SAG Helps in Reducing Brain Edema
Experimental models of TBI in mice have shown that giving SAG can substantially reduce both BBB disruption and brain edema. When SAG is introduced, it boosts the robust nuclear translocation of Gli-1, a downstream signal of Smo activation. This activation sets off a chain reaction that ultimately increases the expression of tight junctions as well as vascular protective factors such as angiopoietin-1 (Ang-1) and tissue inhibitors of metalloproteinase-1 (TIMP-1).
- SAG enhances Gli-1 nuclear translocation, which is linked with robust BBB repair.
- It increases the mRNA expressions of claudin-5 and occludin, essential building blocks for BBB stability.
- The compound also promotes the expression of Ang-1 and TIMP-1, which are key in mitigating BBB disruption.
This multi-pronged effect of SAG is vital because it addresses several of the fine shades that make TBI such a complicated piece. By helping to restore the BBB and controlling inflammatory mediators, SAG may steer the recovery process along a more favorable path.
Sorting Out the Defense Against Neuroinflammation
Neuroinflammation is another overwhelming aspect of TBI. Once the BBB becomes compromised, inflammatory molecules flood into the brain, triggering a cascade of events that can lead to further neuronal damage and chronic deficits. The elevated levels of inflammatory cytokines such as interleukin-1β (IL-1β) and tumor necrosis factor-α (TNF-α) add to the nerve-racking scenario.
Interestingly, both Shh and SAG appear to help dial down the inflammatory response. Laboratory studies indicate that administration of these molecules not only reduces the immediate leakage of serum proteins into brain tissue but also tampers down the expression of cytokines and chemokines. This effect is likely tied to the restoration of BBB integrity and the resultant prevention of pro-inflammatory cell infiltration.
Key Points on Neuroinflammation Control
The following bullet list outlines the main observations from recent studies on neuroinflammation related to TBI:
- Elevated inflammatory markers are a clear sign of TBI-associated neuroinflammation.
- Shh-based interventions have been linked with decreased expression of IL-1β, TNF-α, MCP-1, and MIP-2.
- Smo agonists like SAG are shown to suppress the release of enzymes such as COX-2 and NOS-2 that contribute to further tissue damage.
- Reducing neuroinflammation helps improve both motor and cognitive functions post-injury.
As the research suggests, reducing the levels of these inflammatory mediators is not just about managing symptoms—it is a key step in laying the groundwork for long-term recovery. By tackling the nerve-racking problem of ongoing inflammation, these treatments may ultimately help to reduce the risk of chronic neurological deficits in patients who have suffered a TBI.
The Promise and Pitfalls of Clinical Application
While these findings are encouraging, the translation from lab bench to bedside is often loaded with challenges. The research discussed here has been primarily conducted in animal models, where controlled conditions allow for the careful observation of outcomes following treatment with Shh or SAG. When it comes to human application, several of the hidden complexities and subtle parts of the issue come to the forefront.
For one, dosing strategies need to be fine-tuned. In experimental settings, SAG has been tested at various doses—from 1 mg/kg up to 15 mg/kg—and has shown promising results in mitigating vasogenic edema and neuroinflammation. The ideal dose for humans, however, remains an open question. Research must take into account the fine balance between achieving therapeutic benefits and avoiding potential adverse side effects.
Another challenge is the route of administration. Intravenous (i.v.) injections deliver the drug quickly and effectively into the systemic circulation, but this method may not always be practical or comfortable for patients in real-world settings. Oral administration, as explored in other studies, could offer a less intimidating yet effective alternative, but factors such as the drug’s bioavailability and its ability to cross the BBB when taken orally need further investigation.
Considerations for Clinical Translation
Before these treatments become part of everyday clinical practice, several key points must be addressed:
- Dose-Finding Studies: Further research is needed to determine the optimal dose that maximizes benefits without triggering side effects.
- Safety Profiles: The potential off-target effects of Smo agonists like SAG must be meticulously evaluated in long-term studies.
- Administration Methods: Exploring both i.v. and oral routes will be important to figure out which approach offers the best balance between efficacy and patient comfort.
- Time Windows for Treatment: Early intervention appears to be critical. Treatments started within a few hours after TBI are likely to be more effective, but the ideal treatment window needs to be clearly defined.
These considerations reflect the absolute need for future research to build on the promising findings from pre-clinical models, taking into account the confusing bits of translating dosing regimens, safe administration methods, and timing strategies into clinical work. In the end, the goal is to figure a path that makes these innovative therapies accessible for patients in need.
Impact on Neurological Function and Patient Recovery
Ultimately, the success of any TBI treatment is measured not just by its ability to repair tissue at the microscopic level, but by its impact on overall neurological function. Experimental evidence indicates that treatment with SAG or Shh not only reduces the brain water content—one of the hallmarks of vasogenic edema—but also translates into meaningful improvements in motor coordination and cognitive function.
For instance, animal studies employing rotarod and beam walking tests have shown that animals treated with SAG perform better, regaining motor ability more quickly than those left untreated. More importantly, cognitive tests, such as the novel object recognition test, suggest that these treatments help restore some of the lost cognitive capacity. This integration of improved motor and cognitive outcomes represents a significant breakthrough in a field where progress has been slow and often off-putting.
Real-World Benefits and Long-Term Goals
From a patient’s perspective, the tall order of recovering from TBI carries numerous practical challenges, including issues with memory, balance, and overall functioning. Many of these animal studies provide hope that by targeting the BBB and reducing inflammation, patients might see faster and more complete recoveries. Long-term, such treatments could decrease the burden of chronic neurological deficits that often follow TBI.
To better illustrate the potential benefits, consider this bullet list summarizing the real-world outcomes envisioned from Shh/SAG therapies:
- Reduced brain edema leading to lower intracranial pressure.
- Improved BBB integrity, minimizing the infiltration of harmful substances.
- Decreased neuroinflammation, which in turn could mitigate long-term cognitive and motor impairments.
- Shorter recovery periods and a better quality of life post-injury.
Even though bridging the gap from animal models to human treatments is not without its nerve-wracking twists and turns, the prospect of a treatment that addresses multiple facets of TBI offers substantial optimism for the future.
Working Through the Tiny Details and Hidden Complexities
It is important to acknowledge that while the promise of Shh and SAG is substantial, the research is still in its early stages for clinical application. There are many small distinctions and subtle parts that researchers must continue to investigate. For example, while both astrocytes and brain endothelial cells play a crucial role in Shh signaling, there is still some debate about who really carries the torch, so to speak, in terms of producing and responding to these signals. Some studies suggest that astrocytes are the major source of Shh, while others point to a more distributed role involving the brain’s microvascular cells.
Moreover, the administration of Smo blockers like Jervine in experimental settings has provided insight into the critical role that endogenous Smo plays. By blocking Smo, researchers have observed worsened BBB disruption and increased brain edema—findings that underscore the necessity of a well-functioning Shh-Smo pathway for recovery. These results help to figure a path through the intricate maze of cellular signals and interactions that are part of brain repair.
Addressing the Tricky Parts With Future Research
Future studies should aim to manage the following challenging issues:
- Cell-specific Roles: Clarifying whether astrocytes, endothelial cells, or both are most critical in mediating the effects of Shh.
- Molecular Pathways: Further detailing the signaling cascades downstream of Smo activation, including the nuclear translocation of Gli-1.
- Long-term Outcomes: Investigating whether the observed improvements in acute settings translate into sustained neurological benefits over months and years.
- Comparative Studies: Evaluating the efficacy of Shh versus its small-molecule agonists, such as SAG, to decide which might be more practical for clinical use.
By carefully sorting out these intertwined issues, researchers hope to move from preliminary findings to robust clinical trials in the near future. Only then can we translate these promising strategies into everyday medical practice for the benefit of TBI patients worldwide.
Sorting Out the Road Ahead: Challenges and Optimism
There is no denying that the road ahead is full of problems. Bringing new treatments from the laboratory to clinical use is, by nature, a process loaded with challenges. Still, the early results provide reasons for cautious optimism. The indication that both exogenous Shh and Smo agonists like SAG can reduce vasogenic edema and neuroinflammation marks a significant step forward, offering hope to patients suffering from the devastating consequences of TBI.
We must remember that while these results are promising, the nerve-racking journey through pre-clinical and clinical trials is just beginning. Key aspects—ranging from dosage to administration methods and long-term safety—need to be meticulously resolved. Researchers and clinicians are now focused on finding the best ways to make these treatments accessible and safe for human use. The current body of work lays a strong foundation for the next phase of therapeutic innovation.
Bridging Pre-clinical Success with Clinical Reality
For medical professionals, the translation of these findings into practical, real-world treatments is paramount. Stakeholders in healthcare, including researchers, clinicians, and pharmaceutical companies, must work together to manage the many challenges ahead. This includes:
- Conducting detailed dose-finding studies on humans to mimic the promising results observed in mice.
- Exploring both intravenous and oral administration routes to enhance drug delivery and patient comfort.
- Monitoring for potential off-target effects to ensure that any new therapeutic regimen is as safe as it is effective.
- Ensuring that the compounds can be manufactured and distributed in a cost-effective manner while maintaining high quality.
By sorting out these trickier bits early on, the research community is setting the stage for more robust clinical trials—trials that could herald a new era of TBI care and recovery.
In Conclusion: A Promising New Chapter in TBI Treatment
In summary, the evidence emerging from recent laboratory and pre-clinical studies strongly suggests that targeting the Shh-Smo signaling pathway can be a highly effective strategy for addressing the nerve-wracking challenges posed by TBI. By reinforcing the BBB, reducing vasogenic edema, and calming the cascade of neuroinflammatory responses, both recombinant Shh and small-molecule agonists such as SAG offer a multifaceted approach to brain rescue after injury.
There are still many twists and turns ahead. The path to clinical implementation is filled with intimidating details—from fine-tuning dosage and administration to carefully monitoring potential side effects. Yet, with each new study, researchers are able to dig into and figure a path among the tangled issues that have long impeded progress in this field.
This body of work not only represents a major step forward in understanding how our brains respond to trauma but also paves the way for treatments that could dramatically improve outcomes for patients with TBI. It demonstrates that even when the challenges seem overwhelming, scientific innovation can find its way through the confusing bits and reveal potential cures that were once out of reach.
For those watching these developments with hope and enthusiasm, it is clear that the promise of Shh and its associated therapies may one day transform the treatment of traumatic brain injuries. As we continue to piece together the fine points of this therapeutic puzzle, we must remain dedicated to advancing both our understanding and our clinical practices. The ultimate reward will be a new frontier in which TBI patients can look forward to better recovery prospects and improved quality of life.
Looking ahead, the collaboration between basic science researchers and clinicians will be critical. By combining their hands-on expertise with cutting-edge research, these experts will be able to get around the tricky bits of TBI treatment. They are working hard to ensure that each small distinction and hidden complexity is addressed, so that in the not-too-distant future, patients will benefit from more effective, targeted therapies that not only alleviate the symptoms but also resolve the underlying causes of brain injury.
In this evolving landscape of regenerative medicine, the road to recovery might still be loaded with issues, but the emerging evidence gives us a reason to be cautiously optimistic. With ongoing research and rigorous clinical testing, the hope is that the strategies inspired by Shh and its agonists will soon find their place as a super important part of TBI treatment protocols.
Ultimately, it is the value of these pioneering efforts that reminds us: even in the face of overwhelming challenges, science is constantly evolving, finding ways to take us through the twists and turns toward better care and improved lives for those affected by traumatic brain injuries.
Originally Post From https://faseb.onlinelibrary.wiley.com/doi/full/10.1096/fj.202502571R
Read more about this topic at
Neuroprotective Effects of the Sonic Hedgehog Signaling …
Neuroprotective effects of Sonic hedgehog agonist SAG in …