Introduction: The Dual Challenge of Diabetes and Coronary Artery Disease
Diabetes mellitus dramatically increases the risk of coronary artery disease, creating a scenario where patients are burdened by tangled issues and confusing bits when it comes to interventional procedures. As a prevalent condition, diabetes not only accelerates the formation of atherosclerotic plaques but also creates a more intimidating coronary environment for interventionists. In this opinion editorial, we take a closer look at the evolution of percutaneous coronary interventions (PCI) and the promise of drug-coated balloons (DCB) in diabetic patients—discussing their potential advantages, current evidence, and future directions.
When we talk about coronary interventions, the twists and turns are significant, especially in diabetic populations. Patients with diabetes typically exhibit more diffuse coronary disease, a higher burden of plaque, and an enhanced inflammatory and prothrombotic state—all of which contribute to higher rates of adverse events post-procedure. Although drug-eluting stents (DES) have improved overall outcomes compared to earlier treatments, many of the problematic pieces remain unresolved, primarily in patients with diabetes. This article dives into the fine points of these challenges and examines how DCBs might offer a promising alternative.
Shifting from Drug-Eluting Stents to Drug-Coated Balloons
Over the years, drug-eluting stents have been at the forefront of PCI, reducing revascularization rates and showing improved clinical outcomes in many patients. However, when dealing with the nerve-racking complications of diabetes, even modern DES technology faces several tricky parts. Diabetic patients are prone to recurring restenosis, in-stent thrombosis, and a higher rate of target-lesion revascularization. These stimulating challenges have pushed clinicians and researchers to explore other revascularization strategies.
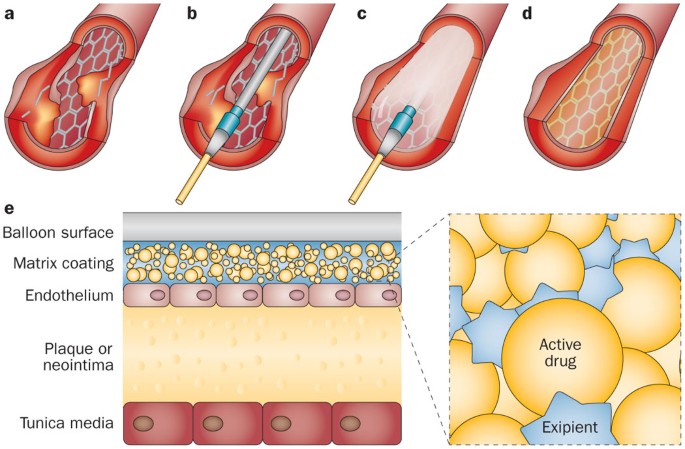
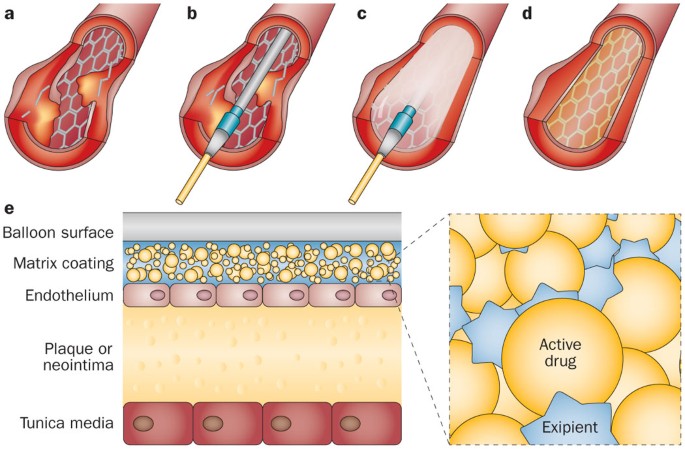
Drug-coated balloons offer a unique approach: they deliver antiproliferative drugs directly to the vessel wall without leaving behind any permanent metallic scaffold. This potential for preserving natural endothelial function, avoiding chronic inflammation, and reducing long-term complications has generated considerable interest in the interventional community. In the following sections, we will dig into how these innovations address the problematic issues associated with traditional DES, especially in diabetic patients.
Diabetes Mellitus and Coronary Artery Disease: Understanding the Underlying Mechanisms
Breaking Down How Hyperglycemia Affects the Heart
Diabetes is known to accelerate coronary atherosclerosis through several intertwined mechanisms. High blood sugar and insulin resistance kickstart a series of biochemical events that lead to the non-enzymatic glycosylation of low-density lipoproteins. This process generates oxidized forms of LDL, which are then taken up by macrophages to form foam cells—the very core of atherosclerotic plaque buildup.
Other key factors include:
- Impaired production of vasodilators such as nitric oxide, leaving the endothelium less capable of adjusting blood flow.
- The proinflammatory environment that increases cytokine activity, leading to vascular injury.
- Exacerbated platelet aggregation, which intensifies the risk of thrombosis.
All these factors combine to create a coronary artery disease presentation that is full of problems, especially in diabetic patients. The vessels tend to be more diffusely diseased, show signs of diffuse calcification, and have higher occurrences of vulnerable, rupture-prone plaques.
The Fine Points of Diabetic Coronary Pathophysiology
For diabetic patients, the little details matter. Endothelial dysfunction, impaired vasodilation, and the overall inflammatory state contribute to a coronary environment that is difficult to manage. These subtle parts add layers of complexity when planning interventions. In practice, the nitty-gritty of diabetic coronary disease means that interventions must account for the additional risks—twisting the usual risk–benefit calculations we employ in non-diabetic individuals.
Examining the Performance of Contemporary Drug-Eluting Stents
Second-generation drug-eluting stents have certainly improved outcomes, but they are not without their limitations. Many clinical studies have noted that even with improved stent platforms, diabetic patients still suffer from higher rates of target-lesion revascularization and restenosis. These results shine a spotlight on the challenging parts of traditional stenting, putting diabetic patients at a disadvantage due to the persistent risk of unfavorable outcomes.
Multiple aspects contribute to these mixed results:
- Delayed endothelial healing: Diabetes often slows the process of endothelial coverage over the stent, leaving it exposed for longer periods.
- Increased thrombotic risk: The prothrombotic state in diabetic patients can lead to an elevated risk of stent thrombosis.
- Neoatherosclerosis: The development of new atherosclerotic lesions within the stented area has been observed to occur more frequently among diabetic individuals.
These complications underline that the current generation of DES may not completely mitigate the short and long-term adverse events associated with stent implantation, urging researchers to explore alternative technologies.
DCB Angioplasty: A Promising Alternative for Diabetic Patients
How Drug-Coated Balloons Work in a Diabetic Environment
Drug-coated balloons take a very different approach compared to stents. They are designed to deliver antiproliferative drugs to the vessel wall without leaving any permanent hardware behind. This strategy has several implications for diabetic patients:
- Preservation of Vessel Function: Without a metal scaffold in place, the natural movement and vasomotion of the artery can be maintained.
- Reduction in Chronic Inflammation: The absence of a foreign body minimizes ongoing inflammatory responses, which is critical in the already loaded coronary environment of a diabetic patient.
- Lower Risk of Stent-Related Complications: Issues such as in-stent restenosis and stent thrombosis are virtually eliminated when no permanent implant is used.
In effect, DCB angioplasty offers a method to sidestep many of the delicate features of restenosis and stent failure, making it an appealing option especially for patients with small vessels or diffuse disease—a common pattern in diabetes.
Comparing Outcomes: DCB Versus DES in Diabetic Settings
Recent comparative studies have provided enlightening insights into the benefits of DCB-based PCI versus DES-based treatments, particularly for diabetic patients. In many investigations, DCBs have demonstrated a lower incidence of target lesion revascularization and a trend toward reduced major adverse cardiovascular events (MACE).
A few key studies highlight these differences:
| Study | Patient Group | Main Outcome | Observations |
|---|---|---|---|
| DARE Trial | Diabetic patients with in-stent restenosis | Comparable lumen diameter and clinical outcomes | DCB showed a trend toward lower complications. |
| DM-Dragon Registry | 473 diabetic patients with ISR | Similar clinical outcomes, lower all-cause death with DCB | DCB improved survival rates. |
| BASKET-SMALL 2 | Small vessel disease in diabetics | Comparable MACE with significantly lower TVR | DCB offered potential benefits in reducing reintervention rates. |
| REC-CAGEFREE I | De-novo CAD in diabetic patients | No significant difference in composite outcomes | Subgroup analysis showed similar performance. |
While results across studies are mixed, the overall trend supports that DCBs can effectively reduce some of the minute details that contribute to poor outcomes in diabetic patients. It is important to note, however, that definitive conclusions can only be drawn with larger randomized controlled trials.
Addressing the Tricky Parts in Diffuse and Multivessel Disease
Diabetic patients frequently present with diffuse coronary artery disease and multiple affected vessels. These are truly nerve-racking scenarios for intervention, given the spread-out nature of lesions and small vessel sizes. Here, DCBs offer a distinct edge:
- Hybrid PCI Strategies: DCBs can be used alone or in tandem with DES—a blended approach—to treat long, diffuse lesions.
- Fewer Metal Implants: By reducing the overall metallic burden in the coronary circulation, DCB use may lower chronic inflammatory responses.
- Preserving Future Surgical Options: In cases where bypass surgery might be needed later, the absence of extensive stent scaffolding can be advantageous.
Studies have shown that when DCBs are used for multivessel disease in diabetic patients, there is a notable reduction in the cumulative risk of major events, including cardiac death and repeated revascularization procedures. This evidence suggests that DCB-based techniques could be a key component in the future management of diabetic coronary artery disease.
Personalizing Treatment: Finding the Right Approach for Diabetic Patients
Diving Into the Individual Needs of Diabetic Patients
One of the most important lessons from recent research is that diabetes is far from a uniform disease. Variability in blood sugar control, duration of disease, and associated complications means that a one-size-fits-all approach does not work. In essence, treating diabetic coronary disease requires a personalized strategy that takes into account:
- Baseline glycemic control and insulin status (whether patients are insulin-treated or not).
- The extent of coronary artery involvement—focal versus diffuse disease.
- The size of the coronary vessel, especially in cases of small-vessel disease where DES may perform less optimally.
- The overall risk profile, including concomitant conditions and other cardiovascular risk factors.
By understanding these subtle details, clinicians can figure a path that may integrate hybrid strategies, combining the advantages of DCBs with traditional stenting when needed. Such individualized planning is essential to manage both the short-term and long-term challenges that come with diabetic coronary disease.
Essential Protocols and Preventive Measures
Alongside the choice of intervention, there are several key preventive measures that are super important for optimizing outcomes in diabetic patients:
- Strict Glycemic Control: Keeping blood sugar levels in check is a foundational requirement to reduce inflammation and further atherosclerotic progression.
- Comprehensive Risk Factor Modification: This includes managing high blood pressure, lipid levels, and ensuring lifestyle modifications such as diet and exercise are in place.
- Antiplatelet Strategies: Proper antiplatelet therapy is crucial to minimize thrombotic complications after the procedure.
- Utilization of New Antidiabetic Treatments: Medications that have proven cardiovascular benefits should be prioritized.
By taking this multi-pronged approach, the confusing bits surrounding the long-term outcomes of coronary interventions in diabetics can be better managed. A well-tailored treatment plan not only addresses the immediate procedural issue but also sets the stage for sustained cardiovascular health.
Expert Perspectives: The Future of DCB in Diabetic Coronary Interventions
Future Clinical Trials and Research Focus
The current body of research suggests that DCBs hold significant promise for overcoming many of the tangled issues associated with PCI in diabetic patients. However, the evidence mainly stems from observational studies and small randomized trials. To solidify the role of DCBs, larger, well-powered clinical trials are essential. These trials should aim to explore:
- The long-term benefits of DCB angioplasty over DES, particularly in stable diabetic patients with diffuse coronary disease.
- The efficacy of hybrid strategies that combine DCB with minimal DES implantation in complex lesions.
- Subgroup analyses that focus on the outcomes of insulin-treated versus non-insulin-treated diabetic patients.
- The comparative impacts on quality of life and mortality, ensuring the measured outcomes translate into real-world improvements.
As future evidence unfolds, clinical practice may shift towards more selective use of DCB-based interventions, carving a niche for these devices in the therapeutic arsenal—especially for high-risk patients.
Benefits and Limitations of the DCB Approach
It is important to weigh both the tangible benefits and potential limitations of drug-coated balloons in the management of coronary interventions in diabetic populations. Here is a clear overview:
| Advantages of DCB | Potential Limitations |
|---|---|
|
|
Despite these limitations, the evidence is steadily accumulating in favor of DCB use for certain diabetic patients—especially those with small vessels or diffuse lesions where conventional DES use may prove suboptimal.
Integrating DCB into Clinical Practice: A Balanced View
Clinicians are now working through the process of managing their way through diverse patient profiles by adopting a balanced approach that integrates both traditional and novel therapies. While drug-eluting stents continue to be a cornerstone of PCI, the addition of DCB-based strategies enables physicians to take advantage of the unique benefits of each modality. For example:
- In small vessel disease, DCBs can offer significant advantages by avoiding the complications of undersized stents.
- In cases of in-stent restenosis, DCBs help avoid repeated stenting and the complications associated with multiple layers of metal.
- In diffuse and multivessel disease, a hybrid approach combining DES for proximal segments and DCB for distal or smaller segments can help optimize outcomes.
By embracing such hybrid strategies, the field of interventional cardiology continues to evolve, providing hope for better long-term outcomes in a patient population that is notoriously challenging due to the nerve-racking repercussions of diabetes.
Essential Considerations When Choosing DCB-Based Interventions
Understanding the Patient’s Unique Profile and Needs
One of the key responsibilities for interventionalists is to figure a path through the maze of patient-specific factors. Diabetic patients are not a homogeneous group—their needs vary based on the duration of diabetes, the degree of glycemic control, and the presence of related complications. When contemplating the use of DCB, doctors need to take these subtle details into account:
- Assessing Vessel Size and Lesion Complexity: Small coronary vessels and diffuse lesions may be better managed with DCB, as compared to stenting with DES.
- Considering the Inflammatory Milieu: A patient with high inflammatory markers might benefit from the reduced chronic inflammation associated with DCB use.
- Evaluating the Risk of Future Revascularization: Patients who may need further interventions, or even coronary artery bypass grafting in the future, can benefit from a strategy that leaves fewer metal implants behind.
These are key factors that contribute to a truly personalized treatment plan. Taking such an individualized approach ensures that the benefits of DCB are maximized while avoiding the potential pitfalls seen in a one-size-fits-all strategy.
The Role of Preoperative and Postoperative Management
Beyond the procedure itself, managing diabetic patients requires a comprehensive approach that begins well before and continues long after the intervention. Preoperative optimization of blood glucose levels, along with meticulous adherence to antiplatelet therapy, is essential. Similarly, postoperative care should involve:
- Regular Follow-Up Assessments: Continuous monitoring using imaging and functional testing can help detect early signs of restenosis or vessel remodeling.
- Aggressive Management of Cardiovascular Risk Factors: This includes lifestyle modifications, blood pressure control, and lipid management.
- Close Coordination with Endocrinology: Ensuring integrated care between cardiologists and endocrinologists can significantly improve overall outcomes.
Integrating these measures helps mitigate some of the nerve-racking challenges that arise from the heavily loaded coronary environment typical of diabetic patients.
Expert Opinions: Charting a New Course in Coronary Treatment
Clinician Insights on the Future Trends for DCB Use
Many experts in the field are optimistic about the role of drug-coated balloons, particularly as further research clarifies their benefits. While current evidence is promising, the call for larger, randomized controlled trials remains loud and clear. Experts believe that:
- The strategic use of DCB will transform the management of complex, diffuse coronary disease in diabetic patients.
- Hybrid approaches that combine DES with DCB will become a standard, especially for multivessel and bifurcation disease.
- Personalized therapy will take center stage, incorporating the use of new-generation antidiabetic medications that have cardiovascular benefits.
The collective sentiment in the medical community is that embracing these innovative approaches will steer through the tangled issues of diabetic coronary intervention and ultimately lead to improved patient outcomes.
Balancing Innovation with Caution
While the potential of drug-coated balloons is certainly exciting, it is essential to approach this innovation with a balanced standpoint. Adopting new technologies requires a careful evaluation of:
- Long-term safety profiles, especially with regards to late lumen enlargement observed in some early studies.
- The variability of drug delivery and absorption in diverse lesion types.
- Crossover risks for patients initially managed with DCB who later require DES implantation due to unforeseen complications.
This balanced perspective ensures that while we celebrate innovation, we do not overlook the need for well-designed, comprehensive studies that address all the fine shades of differences in patient outcomes.
Conclusion: Finding a Path Forward in the Management of Diabetic Coronary Disease
In summary, diabetic patients face an overwhelming risk of diffuse, small-vessel, and multivessel coronary artery disease—a reality that renders conventional PCI using drug-eluting stents limited by its own set of nerve-racking complications. As explored throughout this editorial, drug-coated balloon angioplasty holds considerable promise as a viable, sometimes superior, alternative that directly addresses several of the complicated pieces associated with stent-based therapies.
By offering a means to deliver antiproliferative therapy without leaving behind a permanent metallic implant, DCBs preserve the natural function of the coronary vessel and reduce the long-term inflammatory response. Although the existing research base is primarily derived from smaller studies and observational data, emerging clinical trials and expert insights suggest that DCBs could play a transformative role in the individualized management of diabetic coronary artery disease.
Ultimately, in an era where precision medicine is increasingly recognized as a gamechanger, incorporating DCB technology into clinical practice represents not just an advance in device innovation, but a more holistic move toward addressing the unique, tricky parts and tangled issues that characterize diabetic patients’ cardiovascular health. As ongoing studies and future trials provide more robust data, it is essential for clinicians to remain open to hybrid strategies that combine the strengths of both drug-coated balloons and traditional stenting. This integrated approach ensures that every patient gets a treatment plan that is as unique and complex as their underlying disease—a true step forward in delivering the essential, tailored care that our patients deserve.
In conclusion, the future of coronary intervention in diabetic patients looks promising as we continue to find our way through the maze of clinical challenges. Whether through fully DCB-based strategies or thoughtfully blended approaches with DES, the goal remains clear: to provide safe, effective, and long-lasting treatment outcomes that address the subtle details and nerve-racking twists and turns inherent in diabetic coronary disease management.
As practitioners, researchers, and policymakers work together to generate and evaluate new evidence, it is our hope that the journey toward improved outcomes for diabetic patients will be paved with innovative solutions that align with the reality of their condition. Only then can we claim to have truly mastered the art of finding our path through the tangled issues and complex pieces of coronary artery disease in the diabetic population.
Originally Post From https://cardiab.biomedcentral.com/articles/10.1186/s12933-025-02922-2
Read more about this topic at
Strategies for Multivessel Revascularization in Patients …
Interventional Revascularization of Coronary Artery …