Reassessing PET-CT’s Role in Asymptomatic Polymyalgia Rheumatica Cases
The world of modern imaging is evolving at a nerve-racking pace, and new research is constantly inviting clinicians to figure a path through tricky parts of diagnosing inflammatory conditions. One of the latest studies from Brest University Hospital has shed light on the hidden potential of 18F-FDG PET-CT scans in detecting subclinical giant cell arteritis (GCA) and occult cancers among patients with polymyalgia rheumatica (PMR) who lack overt symptoms. This editorial takes a closer look at the study’s findings, offering observations on how advanced imaging techniques might reshape the way we manage PMR, and it explores the broader implications for patient care.
With chronic inflammatory diseases like PMR, the twists and turns in diagnosing coexisting conditions can be overwhelming. While PMR itself can present a set of confusing bits, the potential for associated risks—such as GCA or hidden cancers—adds another layer of complexity. The study we review today suggests that routine incorporation of PET-CT scans might offer tremendous benefits by uncovering tangled issues before they manifest as clinical emergencies. It is both a timely and thought-provoking piece for clinicians and healthcare policymakers alike.
Emerging Insights: Advanced Imaging as a Diagnostic Tool for Hidden Diseases
During the past few decades, imaging technology has made quantum leaps in its ability to detect diseases at early stages. The use of 18F-FDG PET-CT has been championed in various fields, from oncology to rheumatology, by offering clinicians a window into the body’s metabolic processes. In the context of PMR, PET-CT scanning is emerging as an indispensable tool. Not only does it help identify subclinical GCA—a condition that might otherwise go unnoticed—but it also flags possible malignant lesions, even when patients do not report typical signs or symptoms.
What makes this approach so appealing is its capacity to dig into the little details rather than relying solely on clinical examination. The scan can highlight abnormal FDG uptake in both vascular structures and periarticular regions, offering early clues to medical professionals before symptoms develop into something more severe. This proactive stance is critical because early diagnosis often translates into more effective management and better patient outcomes.
Understanding the Mechanism Behind FDG Uptake
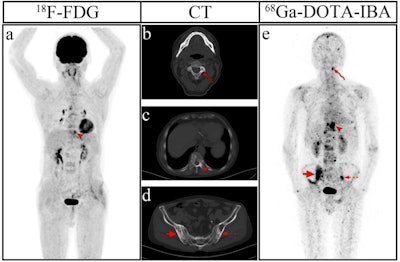
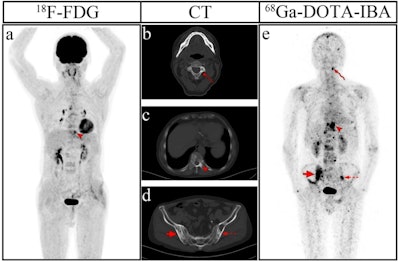
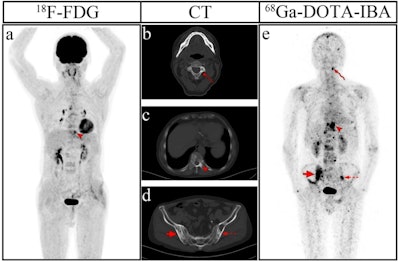
One of the key aspects of the PET-CT scan is the uptake of 18F-fluorodeoxyglucose (18F-FDG) by cells in the body. Areas with high metabolic activity—often a sign of inflammation or malignancy—will take up more FDG relative to normal tissues. In the study, clinicians scored FDG uptake in both vascular and periarticular sites. Suspicious findings, such as vascular uptake graded at 2 or higher, were indicative of subclinical GCA.
This mechanism is important because it not only offers a means to detect hidden inflammation but also provides a snapshot of the overall inflammatory burden in patients with PMR. The findings suggest that a careful interpretation of FDG uptake can act as a beacon for clinicians in identifying patients who may be at risk of developing complications. Moreover, incidental findings of focal FDG uptake could warrant further investigation into possible cancers, whose early detection is absolutely essential for effective treatment.
Observations from the Brest University Study: Data and Reflections
The study in question reviewed 94 PET-CT scans collected between October 2018 and October 2022. These scans were performed on patients aged 50 years or older with confirmed or suspected PMR, divided into new-onset cases and those with treatment failure. The analysis of this patient group provides some striking statistics:
| Finding | Percentage | Group |
|---|---|---|
| Subclinical GCA detection | 10.6% | Overall; 5.3% in new-onset vs. 14.2% in treatment failure |
| Occult cancer detection | 8.5% | Equally distributed between new-onset and refractory cases |
These findings underscore the value of PET-CT scans in uncovering hidden conditions that might otherwise be missed. Among patients with subclinical GCA, the aorta, supra-aortic trunk, and vertebral arteries showed significant uptake. Periarticular regions like the hips, shoulders, ischial tuberosities, and lumbar interspinous bursae also exhibited increased activity. The detailed breakdown helps clinicians piece together the puzzle of PMR’s presentation and its associated risks, providing a clearer picture than routine assessments might reveal.
Key FDG Uptake Patterns in PMR Patients
Let’s break down the data on FDG uptake into clear bullet points to better understand the clinical implications:
- Vascular Uptake:
- Subclinical GCA in 10.6% of patients
- Most common in the aorta (90%), with considerable uptake in the supra-aortic trunk (60%) and vertebral arteries (60%)
- Periarticular Uptake:
- Hips: 95.7%
- Shoulders: 92.5%
- Ischial tuberosities: 79.8%
- Lumbar interspinous bursae: 66.0%
- Incidental Findings of Cancer:
- 8.5% of patients had FDG uptake suggestive of malignancy
- Confirmed cases included prostate, myeloma, endometrial, and gallbladder cancer
Each of these details presents fine points that combine to create a comprehensive approach to managing PMR. For clinicians, being alerted to these hidden complexities means they can take decisive action before complications become overwhelming. This proactive approach is key in addressing the small distinctions in FDG uptake that might differentiate a benign process from something more serious.
Methodological Reflections: Benefits and Limitations
The retrospective, single-center design of the Brest University study brings both strengths and some tangled issues. On one hand, a focused group of 94 scans can offer rich detail and clearer insights into specific patterns of FDG uptake. On the other hand, the study’s narrow scope and limited sample size make it challenging to generalize these results to broader populations. This is a classic case of balancing precise information with the need to account for real-world variability.
While the study opens the door to incorporating PET-CT scans into routine PMR management—especially for patients experiencing treatment failure—the potential for false positives or incidental findings remains a challenge. The possibility of over-diagnosis or unnecessary follow-up procedures is a concern that healthcare providers need to manage carefully. It is a reminder that while technology can shine a light on hidden processes, it also demands careful interpretation and judicious use.
Considerations for Future Research Approaches
Looking ahead, more extensive, multi-center studies are called for to confirm and expand upon these promising results. Future research should aim to:
- Enroll larger, more diverse patient populations
- Explore the cost-effectiveness of routine PET-CT in PMR
- Investigate long-term outcomes in patients detected with subclinical GCA or occult cancer
- Assess optimal protocols for FDG uptake scoring and interpretation
Addressing these points will help dispel some of the intimidating unknowns, making it easier for clinicians to steer through the emerging complexities of PMR and its coexisting conditions. Successfully tackling these challenges is indispensable not only for improving diagnostic accuracy but also for enhancing overall patient care.
Balancing Diagnostic Accuracy with the Overwhelming Data Landscape
In an era where advanced imaging provides a flood of data, clinicians face the nerve-racking task of sorting out what is clinically relevant. The transformative potential of PET-CT lies in its ability to offer a detailed snapshot of the patient’s internal environment. However, the additional information can sometimes be overwhelming, creating more questions than answers.
It becomes necessary to weigh the benefits of early detection against the risks of triggering excessive diagnostic workups. In cases of PMR, where symptoms may already be tangled with other musculoskeletal complaints, the decision to use PET-CT should be based on a careful evaluation of each patient’s unique situation. Here, personalized medicine comes into play, where both the art and the science of medicine merge to achieve optimum patient outcomes.
Strategies for Managing Excessive Diagnostic Data
Clinicians can manage the influx of imaging data by adopting several practical strategies, including:
- Implementing standardized scoring systems: Utilization of clear FDG uptake grading helps in differentiating between benign and concerning findings.
- Collaborative care models: Enlisting the expertise of radiologists, rheumatologists, and oncologists ensures that data interpretations are balanced and informed by multiple viewpoints.
- Regular follow-up imaging: Where needed, planned imaging follow-ups can monitor changes over time rather than prompting immediate intervention based on one scan alone.
- Patient education: Informing patients about the possibilities of incidental findings can allay fears and help set realistic expectations during the diagnostic process.
The integration of these strategies assists healthcare teams in sorting through the overwhelming bits of data and makes it possible to focus on truly critical findings that require prompt action.
Clinical Impact: Early Detection of Subclinical GCA and Hidden Cancers
The early detection of subclinical GCA and incidental cancer findings is a super important step that could reshape patient outcomes in polymyalgia rheumatica. The benefits of early diagnosis in these patients include:
- Prompt intervention: Early identification of inflammation in vessel walls or occult tumors provides the opportunity to initiate treatment sooner, potentially reducing complications.
- Personalized care plans: Knowing the detailed metabolic landscape from a PET-CT scan allows physicians to tailor interventions to each patient’s specific needs.
- Improved survival rates: In cases where malignancies are found early, patients might have access to more effective therapeutic options, increasing survival odds.
Yet, managing potential side effects or complications arising from early treatment requires careful consideration. In this context, PET-CT serves not only as a diagnostic tool but also as a means to guide the subsequent course of action. Given the trickiness of balancing early detection with over-treatment, clinicians are called upon to make informed decisions that incorporate both data and a comprehensive understanding of the patient’s history.
Advantages of a Proactive Diagnostic Strategy
Implementing a routine PET-CT scan strategy for patients with PMR, particularly those who are not responding adequately to treatment, can have several advantages, such as:
- Enhanced risk stratification: Identifying patients at higher risk for GCA or occult cancer enables healthcare professionals to allocate resources and attention where it is most needed.
- Refined treatment pathways: With clearer imaging data, treatment strategies can be better aligned to address both the primary symptoms of PMR and any emergent secondary complications.
- Reduction in emergency interventions: Early intervention can help prevent emergencies that are both physically and emotionally nerve-racking for patients.
While some may view the necessity of routine PET-CT scans as intimidating given the additional costs and resource allocation, the potential for improved patient outcomes makes it a discussion that is both timely and super important.
The Broader Clinical Picture: Weighing Risks, Costs, and Opportunities
When considering the widespread adoption of PET-CT scans in managing PMR, it is critical to weigh benefits against potential pitfalls. The hidden complexities of PMR are only part of the equation. Clinicians must also consider the risks of radiation exposure, the overall costs of high-end imaging, and the possibility of incidental findings that might lead to cascading diagnostic procedures.
This balance is laden with challenges. Here are some key considerations:
- Cost-effectiveness: While PET-CT scans provide invaluable diagnostic insights, their routine use must be examined in the context of healthcare budgets. However, preventing complications in the long run might justify the initial expense.
- Patient safety: The minimal risk of radiation exposure should always be factored into the decision-making process, especially for older patients who might be more vulnerable.
- Resource allocation: In community or resource-limited settings, implementing such advanced imaging protocols may require rethinking priorities and investing in training healthcare professionals to figure a path through these complicated pieces.
Healthcare systems must work towards strategies that allow for the integration of PET-CT into standard care protocols for PMR without overwhelming either the patient or the physician with the nerve-wracking additional data. Such an approach ideally balances resource use with clinical benefit—a complex undertaking that remains very much on the edge of current practice standards.
Opportunities for Collaborative Healthcare Models
Multi-disciplinary care models can play a pivotal role in ensuring that PET-CT scans are used effectively. By combining the expertise of rheumatologists, radiologists, oncologists, and primary care providers, the following advantages may be achieved:
- Shared decision-making: Engaging a team to jointly interpret scan findings can help smooth out the rough edges in diagnosis.
- Streamlined follow-up care: A coordinated approach can minimize delays in subsequent treatments or further diagnostic testing.
- Enhanced patient trust: Transparent communication and collaborative care foster a greater sense of security among patients, making them less likely to feel overwhelmed by complicated test results.
Working together, these professionals can turn potentially intimidating new data into actionable information, ensuring that each patient receives care that is both personalized and precisely targeted.
Patient Considerations and the Future Value of PET-CT in PMR
For patients living with polymyalgia rheumatica, chronic pain and fatigue can already be overwhelming. Adding an additional layer of investigative imaging might feel off-putting or even scary. However, the potential benefits of a proactive imaging strategy must not be underestimated. Early detection of subclinical GCA or hidden cancers can mean the difference between rapid intervention and progressive disease that is harder to control.
When patients are informed about the advantages and possible limitations of PET-CT, they can become partners in their own care. Education plays a key role: understanding that a PET-CT scan might unveil important hidden details rather than simply adding complexity can empower patients to make more informed decisions about their treatment options.
Several points warrant special attention for patient-focused discussions:
- Communication: Clear explanations about what PET-CT scans are and what they can reveal help dispel myths and manage expectations.
- Shared risk-benefit analysis: Patients should be encouraged to discuss the potential risks (such as radiation exposure) alongside the benefits of early detection, ensuring informed consent.
- Quality of life considerations: Early diagnosis alone does not solve all problems; however, it can open the door to tailored treatment strategies that significantly enhance life quality.
Considering these factors, it is clear that PET-CT imaging holds a position of promise in the realm of PMR management. Its integration into routine practice, particularly for those patients who do not experience a robust response to initial therapy, could lead to outcomes that are not only clinically better but also more satisfying for patients seeking reassurance in their treatment journey.
The Future of Patient-Centered Diagnostic Strategies
Looking forward, integrating advanced imaging such as 18F-FDG PET-CT with emerging digital health tools and personalized medicine approaches could further refine the way we manage conditions like PMR. Potential areas of innovation include:
- Developing robust algorithms that combine patient demographics, scan data, and clinical features to predict adverse outcomes.
- Using artificial intelligence (AI) to assist radiologists in interpreting subtle FDG uptake patterns.
- Implementing telemedicine consultations that allow multi-disciplinary teams to review complex cases in real time.
These innovations might help ease the tricky parts associated with interpreting the overwhelming data provided by high-end imaging, offering patients a clearer path through the heady array of diagnostic information.
Conclusion: Shaping the Future of PMR Management
The findings from the Brest University study force us to take a longer, more thoughtful look at how diagnostic tools like 18F-FDG PET-CT can address the tangled issues hidden beneath the surface of polymyalgia rheumatica. By detecting subclinical GCA and incidental cancers, PET-CT emerges as an essential diagnostic adjunct in special cases—especially among patients experiencing treatment failure.
Certainly, adopting routine advanced imaging in PMR management is not without its challenges. There remain intimidating questions about cost, over-diagnosis, and the interpretation of a vast amount of data. However, by leaning on collaborative care models, standardized interpretation protocols, and patient education, clinicians can make their way through these complicated pieces with greater clarity.
Polymyalgia rheumatica has long been known for its confusing bits and daunting clinical presentation. The study encourages a proactive approach—one where careful attention to subtle FDG uptake patterns can alert healthcare providers to hidden risks and ultimately save lives. As more research confirms these early observations, it is likely that PET-CT will become a key component in the diagnostic workup for PMR, complementing clinical evaluations and enabling earlier therapeutic interventions.
Ultimately, the integration of advanced imaging is not just about gathering data—it is about making informed decisions that consider the entire patient. In a world filled with nerve-racking twists and turns, using every tool at our disposal can help simplify the tangled pathway to proper diagnosis and effective treatment. With the promise of early intervention and improved outcomes, the case for incorporating PET-CT scans into routine PMR care becomes even more compelling.
As we look to the future, the onus is on both the clinical community and healthcare policymakers to continue researching, refining, and implementing these innovative diagnostic strategies. Only then can we truly turn the tide on the subtle, often hidden, dangers that lurk behind conditions like PMR, ensuring that every patient receives care that is as precise as it is proactive.
By embracing the potential of PET-CT in identifying subclinical GCA and incidental malignancies, we are not only enhancing our diagnostic arsenal but also taking a significant step toward personalized, patient-centered care. In doing so, we affirm our commitment to staying ahead of the curve, even when the pathway is complex and full of problems. The study from Brest University Hospital serves as a reminder that with the right tools and collaborative expertise, even the most intimidating diagnostic challenges can be managed—and ultimately overcome.
Originally Post From https://www.rheumatologyadvisor.com/news/pet-ct-detects-gca-and-cancer-in-asymptomatic-pmr/
Read more about this topic at
NCDs – The SilentKillers
New Apple watch now detects health condition known as …