Understanding Cryptogenic Hemoptysis and Its Clinical Implications
Cryptogenic hemoptysis is a puzzling condition where patients cough up blood with no obvious cause. Although it may seem harmless in some cases, the unpredictable nature of this bleeding can quickly become a nerve-racking scenario. It is essential to take a closer look at the condition and understand its clinical importance in order to offer effective solutions.
In many hospitals, cryptogenic hemoptysis constitutes a significant portion of emergency cases requiring immediate intervention. Despite the absence of classic lung lesions on imaging studies, patients can present with anything from minor bleeding to episodes of life-threatening blood loss. These episodes are not only overwhelming, but they present several tricky parts that challenge even the most experienced clinicians.
It is important to note that without a clearly identifiable cause based on routine diagnostic tests, the management of cryptogenic hemoptysis must rely on both clinical intuition and advanced interventional techniques. One increasingly popular treatment modality that has gained recognition is bronchial artery embolization (BAE), which has the potential to halt the bleeding quickly and with minimal complications.
Bronchial Artery Embolization: A Game-Changer in Managing Hemoptysis
Bronchial artery embolization (BAE) has emerged as an effective intervention to manage hemoptysis, especially in cases where traditional diagnostic imaging fails to identify a specific cause. This treatment is based on the principle of obstructing the abnormal blood flow in the bronchial arteries, thereby stopping the bleeding. The success of BAE has been documented in various clinical studies, showing both short-term efficacy and long-term safety when performed by experienced specialists.
A common approach at several leading institutions involves using a gelatin sponge (GS) as the embolic material. GS is not only cost-effective, but it has a long track record of use in vascular procedures, making it a trusted tool for clinicians who need to quickly figure a path through the challenges posed by active hemoptysis.
One of the appealing aspects of BAE is its adaptability. Doctors can use a super-selective embolization technique to target only the responsible arteries while preserving blood flow to the rest of the lung. This careful selection is crucial when one considers the hidden complexities of the bronchial tree and the need to keep collateral circulation intact.
Intricate Details of the Super-Selective Embolization Technique
The dash into super-selective BAE has revolutionized the treatment landscape for cryptogenic hemoptysis. By diving in with precision, interventional radiologists and pulmonologists are now able to navigate the tiny, convoluted routes of the bronchial arteries with improved clarity and safety.
During the procedure, doctors use microcatheters and microguidewires to closely approach the bleeding site. This method ensures that the gelatin sponge is delivered directly to the problematic vessel, avoiding the unintended blockage of adjacent arteries. The precision of this technique is especially important in avoiding severe complications, such as spinal cord ischemia, which can be one of the most intense and off-putting risks associated with BAE if not managed correctly.
Below is a table that outlines the key steps in the super-selective embolization technique:
| Step | Description |
|---|---|
| Pre-procedural Imaging | Contrast-enhanced CT and, if needed, bronchoscopy to pinpoint the bleeding site. |
| Arterial Access | Femoral arterial access is commonly used with a 4- or 5-Fr vascular sheath. |
| Selective Catheterization | Guiding catheters and microcatheters are used to navigate to the culprit bronchial artery. |
| Embolization | Injection of a gelatin sponge, sometimes in combination with PVA particles, to block the vessel. |
| Post-procedural Assessment | Angiography confirms the achievement of immediate hemostasis and proper embolization. |
This table summarizes the well-practiced procedure, highlighting how each phase contributes to both immediate and sustained control over the bleeding.
Evaluating the Long-Term Efficacy of Gelatin Sponge Embolization
The long-term outlook after bronchial artery embolization with gelatin sponge is generally positive. In several retrospective analyses, patients have shown high recurrence-free rates over a span of months and even years. Recurrence-free rates have been reported as high as 86% beyond the one-year mark, with most patients achieving immediate control of the bleeding after the procedure.
Data collected from clinical studies have demonstrated that gelatin sponge embolization is not just effective for short-term bleeding control but also holds up well in the long run. This is particularly reassuring given that cryptogenic hemoptysis can sometimes reappear in subtle ways—a situation that demands follow-up and occasionally even a second round of embolization if the bleeding recurs.
Some highlights of long-term efficacy include:
- High immediate technical success with complete vascular occlusion.
- Low incidence of severe complications, such as spinal cord injury.
- Effective management even in cases where the initial bronchial artery size is less than 2 mm.
These points show that despite the tiny twists and turns of the bronchial vascular system, BAE with GS remains a reliable and safe procedure.
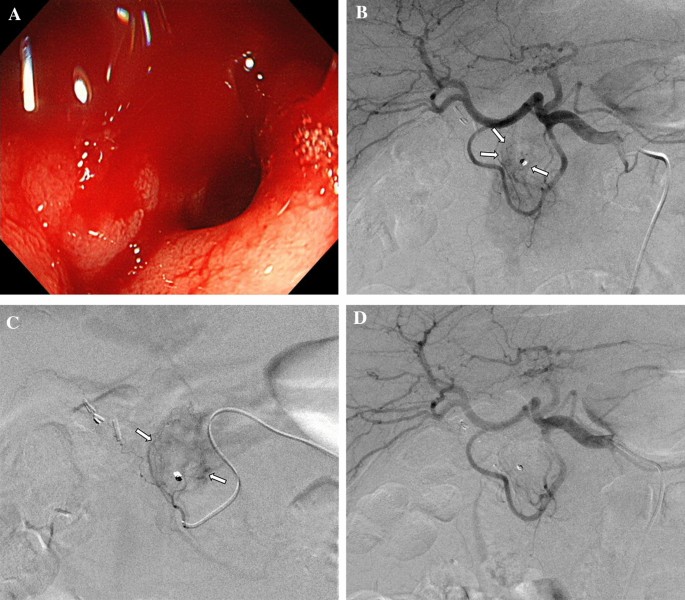
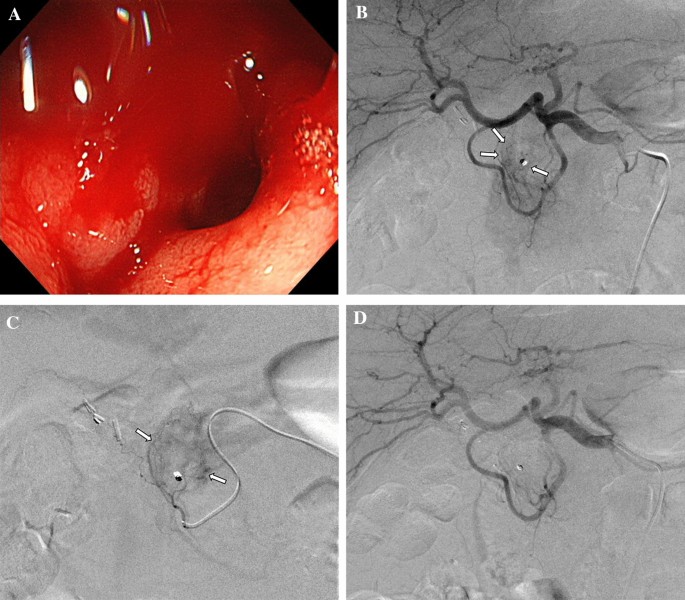
Clinical Insights: Angiographic Findings and Their Impact
Angiography plays a key role in mapping out the vascular supply related to the bleeding sites. It offers clinicians a peek at the fine points that can guide the intervention. In studies conducted over a span of twelve years, angiographic findings consistently revealed traits such as vascular tortuosity, hypervascularity around the bleeding area, and even the presence of microaneurysms in some patients.
These detailed images empower clinicians to make informed decisions during the procedure. For instance, pinpointing a pseudoaneurysm can be particularly important because of its potential to spur recurring hemoptysis. In such cases, additional care is necessary to ensure that the embolic material reaches the exact problematic vessel without spilling over to healthy tissue.
A summary list of key angiographic features includes:
- Vascular Tortuosity: Indicates twisted and looping arteries that may require careful catheter navigation.
- Peripheral Hypervascularity: Suggests increased vessel formation around the bleeding site.
- Microaneurysm Formation: Small dilations that can be linked to recurring bleeding episodes.
- Systemic-Pulmonary Shunts: Abnormal connections that can complicate the clinical picture.
Clinicians must skillfully manage these confusing bits of vascular anatomy to ensure the success of BAE, as the presence of such signs can often signal that the patient is at a higher risk for future bleeding episodes.
Addressing the Challenges: Comparing Intubated vs. Non-Intubated Cases
One notable finding in the clinical literature is the difference between patients who require intubation and those who do not. Intubation is usually reserved for cases with massive hemoptysis, where the bleeding volume exceeds 200 mL in 24 hours and poses an immediate danger to the airway.
Interestingly, studies have shown that there is no significant difference in the long-term recurrence-free rates between intubated and non-intubated patients. Although the intubated group often experiences a more intimidating initial course and stays in the hospital for a longer period, the overall efficacy of the embolization technique remains robust, regardless of the initial severity of the bleeding.
An analysis of patient subgroups reveals the following:
- Intubated Patients: Generally have massive hemoptysis, longer hospital stays, and a need for immediate airway protection.
- Non-Intubated Patients: Present with lower volumes of bleeding and typically have a faster recovery after BAE.
When comparing these two groups, the data suggest that while the immediate clinical picture might be tense and full of problems, proper intervention with BAE tends to level the playing field over the long term. This finding is critical for clinicians as it underscores that even severe cases with intubation can be managed with a positive outlook if treated appropriately.
Safety Profile and Minimizing Risks: Avoiding Spinal Cord Ischemia
Safety is a top concern when it comes to any invasive procedure, and BAE is no exception. One of the most nerve-racking risks associated with BAE is the possibility of spinal cord ischemia. This severe complication typically arises due to accidental embolization of arteries that supply the spinal cord, leading to potentially permanent neurological deficits.
However, the data indicate that with meticulous super-selective catheterization, the risk of spinal cord ischemia can be kept remarkably low. Many institutions have reported rates as low as 0.19% in large-scale studies, which helps to alleviate concerns over this intimidating complication. More importantly, by carefully observing angiographic details and using protective techniques, interventionalists can steer through this challenge effectively.
Safety measures commonly in place include:
- Pre-procedural review of anatomical variations using CT angiography.
- Real-time monitoring during embolization to ensure no backflow into critical vessels.
- Using a combination of embolic materials if necessary to precisely control the extent of occlusion.
These steps are not only super important for patient safety but also instill confidence in both the treating team and the patient that the therapy will be executed without significant risks.
Weighing the Pros and Cons: An Opinion on Gelatin Sponge versus Other Embolic Agents
In recent years, there has been discussion within the medical community about the use of alternative embolic materials like metal coils, N-butyl cyanoacrylate (NBCA), and polyvinyl alcohol (PVA) particles in BAE procedures. Each of these has its own set of benefits and potential pitfalls. However, the use of a gelatin sponge remains a widely accepted practice, primarily for its ease of use, cost-effectiveness, and reassuring safety profile.
When comparing gelatin sponge with alternative agents, several factors come into play:
- Cost and Accessibility: Gelatin sponge is inexpensive and widely available in most medical settings.
- Absorption and Temporary Occlusion: GS is gradually absorbed within 2–6 weeks, offering a temporary solution that can be advantageous when treating unexpected bleeding episodes.
- Clinical Experience: The longstanding history of GS use provides clinicians with a wealth of practical knowledge and experience.
- Recurrence Rates: Studies have reported low recurrence rates with GS, indicating that it is effective even as a temporary agent.
These points illustrate that while alternative materials might provide permanent solutions in certain cases, the gelatin sponge is a reliable option for managing cryptogenic hemoptysis—a condition that often requires quick but careful judgment in the operating room.
Practical Considerations: Guidelines and Operator Experience
The success of BAE in cryptogenic hemoptysis is not solely dependent on the technical aspects of the procedure; the operator’s skill and experience play a crucial role as well. In many institutions, the procedure is performed by teams that include both pulmonologists and interventional radiologists, allowing them to combine their expertise in managing both the unforeseen bleeding and the delicate anatomy of the bronchial arteries.
It is also essential to have clear protocols in place to manage the various tricky parts associated with the procedure. For example, guidelines suggest that the use of pre-procedural CT imaging, followed by a detailed angiographic study, can help in predicting which patients might need more careful management. This collaborative approach often results in higher success rates and fewer complications overall.
Below is a bulleted list of operational best practices:
- Ensure comprehensive pre-procedural imaging to identify all potential sources of bleeding.
- Use super-selective catheterization to minimize the risk of non-target embolization.
- Monitor for any signs of spinal cord involvement during the procedure.
- Maintain a multidisciplinary team approach for optimal decision-making.
- Implement strict post-procedural follow-up to catch and manage any early signs of recurrence.
Adhering to these practical guidelines is not only critical to the immediate success of the intervention but also helps maintain a high standard of care throughout the patient’s recovery process.
Patient Outcomes and Follow-Up: A Close Look at Recurrence Rates
The follow-up phase after BAE is as important as the procedure itself. Patients who undergo BAE for cryptogenic hemoptysis are typically monitored over months and even years to ensure that the risk of recurrence remains low. Although a small percentage of patients may experience a minimal amount of rebleeding, these instances are often managed with either a repeat embolization or conservative treatment using oral hemostatic agents.
The overall recurrence-free rate stands impressively high, with studies reporting close to 100% in the immediate month following the procedure and maintaining a rate of around 86% or higher beyond the one-year mark. It is these long-term outcomes that underscore the strength of BAE with gelatin sponge as a treatment modality for cryptogenic hemoptysis.
In some cases, patients have even experienced minor recurrences that were effectively managed without additional invasive procedures. For example, instances where a patient noticed a small streak of blood in the sputum were resolved with the use of oral medications, rather than resorting immediately to a second embolization.
This data strongly supports the opinion that BAE with GS helps to secure a stable recovery period for patients, offering not just immediate but also persistent relief from cryptogenic hemoptysis.
A Look at the Broader Context: Alternative Perspectives and Future Directions
While the evidence supporting the use of gelatin sponge in BAE is compelling, it is important to appreciate the evolving landscape of embolization therapies. With continuous advancements in material science and interventional techniques, more tools are becoming available to clinicians. Future studies might compare the gelatin sponge with newer embolic agents, such as advanced polymer microspheres, to determine whether even greater efficacy and safety can be achieved.
This forward-thinking approach invites the medical community to continuously re-examine established practices. By poking around in both the successes and the minor setbacks of current treatments, practitioners can work to refine techniques and protocols. Many believe that the future of embolization therapy lies in personalized treatment plans that take into account the specific vascular anatomy and clinical profile of each patient.
Some future areas for research include:
- Comparative studies of GS with permanent embolic agents in diverse patient populations.
- The development of advanced imaging protocols to better predict vascular behavior during BAE.
- Exploring combination therapies that use multiple embolic agents for more complex cases.
- Research into personalized approaches that tailor BAE procedures to the patient’s unique angiographic profile.
By staying informed about these developments, clinicians can continue to offer treatments that are not only effective in the short term but also provide sustainable benefits in the long run.
Real-World Impact: How BAE Changes the Treatment Experience
From a patient-centered perspective, the use of bronchial artery embolization with gelatin sponge has significantly reshaped the treatment experience for those suffering from cryptogenic hemoptysis. Previously, patients with sudden, overwhelming bleeding might have required more invasive surgeries, which could be both intimidating and laden with risks. Today’s minimally invasive techniques offer a super important alternative that is both safer and quicker.
Here are some of the real-world benefits observed:
- Reduced Hospital Stay: Patients generally experience shorter hospitalizations due to the rapid control of bleeding.
- Improved Comfort and Safety: The minimally invasive nature of the procedure reduces discomfort and the risk of long-term complications.
- Quick Return to Daily Life: With effective control of symptoms, many patients are able to return to their routines faster.
- Enhanced Confidence in Treatment: The low recurrence rates and absence of severe complications build trust in the procedure among patients and caregivers alike.
These benefits underscore the importance of having efficient interventional techniques available, which can make a critical difference in emergency settings where every minute counts.
Expert Opinions: Weighing the Clinical and Practical Benefits
Experts in the fields of pulmonology and interventional radiology have weighed in on the merits of using gelatin sponge for BAE. In their opinions, the procedure not only addresses the immediate threat of bleeding, but it also offers a practical and manageable solution for this full-of-problems condition.
Many clinicians appreciate the straightforward nature of GS embolization. Its predictable absorption and cost-effectiveness mean that hospitals can offer this treatment without needing expensive equipment or materials. Moreover, the extensive clinical experience accumulated over the years provides a solid foundation for current practices. The following points summarize expert opinions:
- Clinicians value the balance between efficacy and safety, noting that the complication rate is very low.
- The temporary occlusion provided by gelatin sponge is often enough to allow the natural healing processes to take over, preventing future episodes of bleeding.
- Even in cases with complicated vascular anatomy, the super-selective approach has largely overcome the tricky parts inherent to bronchial embolization.
- Many experts stress the importance of interdisciplinary collaboration, as the combined insights of pulmonologists and radiologists are crucial to a successful outcome.
In summary, these clinical insights support a growing consensus that BAE using GS is a safe and effective treatment that can be widely adopted for cryptogenic hemoptysis.
Clinical Decision-Making: Assessing Patients for Bronchial Artery Embolization
Deciding on the correct intervention for patients with cryptogenic hemoptysis involves a thorough review of multiple factors. While imaging studies provide a wealth of information on the hidden details of the bronchial arteries, additional clinical variables must also be considered. These include the patient’s overall clinical status, the severity of the bleeding, and any underlying comorbid conditions that could complicate treatment.
Physicians are encouraged to work together to ensure that all relevant information gets factored into the decision-making process. This team-based approach helps mitigate the risks of the procedure, while also ensuring that the benefits of BAE are maximized.
A simplified outline of the decision-making process can be presented as follows:
- Step 1: Evaluate the severity of hemoptysis (mild, moderate, or massive) using standard clinical criteria.
- Step 2: Use contrast-enhanced CT scans and bronchoscopy to identify the likely source of bleeding.
- Step 3: Assemble a multidisciplinary team to discuss the patient’s case and weigh the risks and benefits of performing BAE.
- Step 4: Plan the intervention, being mindful of the fine details in the angiographic findings that might affect the choice of embolic material and technique.
- Step 5: Implement the BAE procedure with a focus on avoiding inadvertent embolization of non-target vessels.
- Step 6: Follow up with the patient in the post-procedure period to monitor for recurrence or complications.
This structured approach ensures not only a safe procedure but also a more predictable long-term outcome, which is critical for patients dealing with such a challenging and overwhelming condition.
Final Thoughts and Future Perspectives
In conclusion, bronchial artery embolization using a gelatin sponge has emerged as a highly effective treatment option for managing cryptogenic hemoptysis. Despite the confusing bits inherent in vascular anatomy and the nerve-racking potential of severe bleeding, BAE has proven its worth as a super important tool in modern medicine. The evidence supports its use in both massive and moderate cases, with long-term recurrence rates remaining impressively low.
As we continue to figure a path through the twists and turns of this complex condition, it is clear that future innovations and ongoing research will further refine these techniques. The integration of advanced imaging, improved embolic materials, and a multidisciplinary approach will undoubtedly lead to even better patient outcomes over the coming years.
With ongoing trials and a steady improvement in interventional expertise, the prospects for managing cryptogenic hemoptysis are brighter than ever. It is not unusual for clinicians to look back on years of practice and recognize that the simple act of stopping bleeding is both critical and life-changing for patients. This progress reinforces the idea that sometimes the best solutions are found by returning to tried-and-tested methods—enhancing them with a dash of modern innovation.
The journey to perfecting BAE is a continuous one, filled with both achievements and moments where the medical community needs to dig into the subtle parts of what makes each patient unique. By taking a closer look at not only the scientific data but also the experiences of those on the frontlines, we can ensure that our approach to this full-of-problems condition remains as effective and safe as possible.
In our evolving healthcare landscape, it is essential to manage your way through the tangled issues of cryptogenic hemoptysis with both scientific rigor and compassionate care. The transformation from a once overwhelming emergency to a manageable clinical condition is a testament to the power of multidisciplinary teamwork and persistent innovation in modern medicine.
Ultimately, the use of bronchial artery embolization with gelatin sponge sets a high standard for treating cryptogenic hemoptysis. It provides hope and reassurance to patients who face this intimidating condition, affirming that even when faced with complicated pieces and challenging clinical scenarios, effective and safe treatment options are available.
As research continues and clinical techniques advance, both patients and clinicians alike stand to benefit from further improvements in at-home care and hospital-based interventions. It is a reminder that in the realm of medical science, the dedication to short-term results and long-term outcomes is a journey that never really ends but always strives for better, safer, and more personalized patient care.
Originally Post From https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-025-03948-8
Read more about this topic at
Hemoptysis: Evaluation and Management
A systematic approach to the management of massive …