Opinion: Long-Term Endovascular Management in MALS – Insights from a Challenging Journey
The management of large superior mesenteric artery (SMA) aneurysms secondary to median arcuate ligament syndrome (MALS) has been a topic of heated debate and careful consideration among clinicians. Over the years, endovascular embolization has emerged as a popular treatment option for these cases due to its less invasive nature. However, the journey is filled with tricky parts and tangled issues—a winding path full of complicated pieces, as illustrated in the long-term case of a patient whose vascular anatomy was altered by MALS and complicated further by orthopedic implants. In this opinion editorial, we take a closer look at the twists and turns of managing such cases, sharing insights on imaging challenges, collateral circulation, and the patient’s perspective on treatment choices.
The discussion herein is not only a reflection on technical efforts in endovascular management but also an exploration of the patient-centered decision-making process. With medical options available being both promising and off-putting in their own rights, we dive in to understand the finer details that continue to shape contemporary treatment choices.
Understanding MALS and Its Impact on Vascular Health
Median arcuate ligament syndrome (MALS), sometimes referred to as Dunbar syndrome, is a rare vascular condition where the median arcuate ligament compresses the celiac trunk. This compression leads to altered visceral blood flow, promoting the formation of collateral channels that often expose patients to the risk of developing aneurysms in vessels such as the SMA. Though MALS routinely presents with rather nonspecific gastrointestinal symptoms like post-meal pain, nausea, or unexplained weight loss, its ramifications on arterial health are both crucial and super important to recognize.
When the celiac trunk is compromised, blood flow is rerouted through collateral routes. This compensation, while lifesaving, can also stress the vessel walls, causing dilatation and, ultimately, aneurysm formation. In many cases, these aneurysms develop in the pancreaticoduodenal arcade, although the SMA may also be affected. This shifting of blood dynamics means that any established aneurysm is not simply a bystander; it is a constant threat that demands careful monitoring and timely intervention, especially since even small aneurysms carry a significant risk of rupture.
A brief table summarizing key aspects of MALS and its complications might help clarify:
| Feature | Description |
|---|---|
| Etiology | Compression of the celiac trunk by the median arcuate ligament |
| Common Symptoms | Postprandial epigastric pain, nausea, vomiting, weight loss |
| Collateral Circulation | Increased blood flow through alternative pathways leads to vascular stress |
| Aneurysm Formation | True aneurysm formation in visceral arteries, notably in the pancreaticoduodenal arcade or SMA |
The development of aneurysms under these conditions is an undeniable feature that clinicians must approach with both caution and creative therapeutic strategies. The challenge here is to understand the subtle parts of the vascular changes while balancing the risks and benefits of treatment options.
Patient Perspectives and the Tricky Parts of Endovascular Embolization
One of the overarching themes in managing complex vascular cases like these is the importance of respecting patient autonomy. In the case under discussion, an 80-year-old patient not only faced a slowly growing aneurysm but also chose to decline the option of surgical intervention. Instead, a series of staged endovascular embolizations were undertaken. This decision, while leaving clinicians with its own set of complicated pieces to solve, underscored the necessity of shared decision-making in an era where treatments—even minimally invasive ones—can feel overwhelming and nerve-racking to patients.
The patient’s stance invites us to consider the following points:
- Informed Consent: Clearly explaining the finer details of potential outcomes, success rates, and possible complications is a must-have step in any treatment plan.
- Risk Tolerance: Every patient has their own threshold when it comes to surgical procedures and repeated interventions. Here, the endovascular approach was chosen due to its promise of lower complication rates and quicker recovery times.
- Long-Term Commitment: Endovascular treatment is not always a “one-and-done” procedure. Repeated embolizations may be necessary, a fact that patients must both understand and agree to in practice.
It is essential for clinicians to listen carefully and guide patients through these tangled issues, staying mindful of both the technical limitations and the personal considerations that might sway a patient’s decision. Endovascular embolization, while often effective, can be full of problems when residual perfusion or recanalization occurs, as was evident when the aneurysm in this case stubbornly refilled despite multiple interventions.
The Tricky Parts of Imaging in the Face of Orthopedic Artifacts
One of the most confusing bits of the management of these cases arises from the challenges in imaging. In our patient’s scenario, the presence of bilateral hip arthroplasties and previously implanted embolization coils created significant artifacts. These imaging artifacts have a profound effect, making it difficult to accurately assess the aneurysm size, the degree of embolization, or any potential recanalization.
Magnetic resonance imaging (MRI) would typically be the gold standard for soft tissue evaluation, but metal implants can render the results far from ideal. Instead, clinicians are forced to rely on computed tomography angiography (CTA) and Doppler ultrasound, both of which come with their own set of limitations. These available options, while useful, are a far cry from the clarity that might be anticipated in cases without such interference. This scenario forces clinicians to figure a path through significant limitations and ask, “How much can we trust these images?”
To better organize this discussion, consider the following bullet list of imaging challenges:
- Metal Artifacts: Orthopedic implants can distort the imaging field, limiting the evaluation of aneurysm details.
- CTA Limitations: Although CTA is valuable, it too is prone to artifact interference and may not clearly depict recanalization.
- Ultrasound Hurdles: Doppler ultrasound, while non-invasive, is operator-dependent and may miss subtle flow changes in the aneurysm sac.
- Need for Innovative Techniques: Improved imaging methods, perhaps involving advanced artifact reduction technology, are needed to provide better follow-up data.
These technical issues are not minor; they are central to determining whether further embolization is necessary. When imaging is loaded with issues, each treatment decision must be weighed against the discord between what the technology shows and the patient’s clinical picture.
Collateral Circulation: A Key Player in Treatment Dynamics
A critical element in the management of MALS-related aneurysms is the role of collateral circulation. With the celiac trunk being largely occluded due to MALS, alternative blood flow routes become super important. Specifically, the SMA and its network of branches become more pronounced as they work to supply vital organs like the liver, spleen, and pancreas.
This shift in blood flow dynamics introduces several little twists that clinicians must manage. On one hand, robust collateral circulation is beneficial because it serves as a backup when primary vascular routes fail. On the other hand, the same compensation can trigger the development of aneurysms due to prolonged vascular stress. It is a classic double-edged sword scenario that requires continuous monitoring and an agile treatment plan tailored to the patient’s evolving anatomy.
Below is a simple table summarizing the implications of collateral circulation in the context of MALS:
| Aspect | Implication |
|---|---|
| Positive Role | Maintains blood supply to vital organs despite arterial occlusion |
| Negative Role | Increased flow may lead to vascular wall stress and subsequent aneurysm formation |
| Treatment Impact | Embolization procedures must consider collateral pathways to avoid compromising organ perfusion |
The key here is to strike a balance between ensuring that the aneurysm is effectively managed while still preserving enough collateral flow to maintain organ health. This balancing act can sometimes feel like working through a maze of twists and turns, where every decision may have unintended consequences.
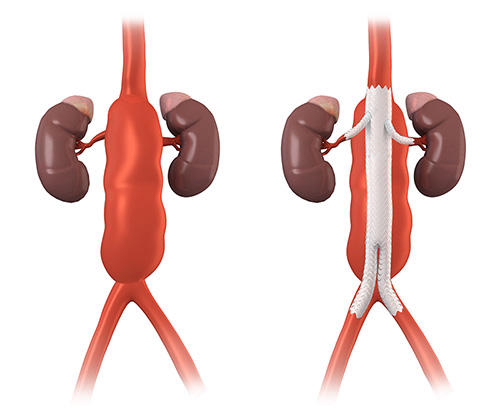
Strategizing Endovascular Embolization Amidst Twists and Turns
The case under discussion illustrates that endovascular treatment for aneurysms in patients with MALS is not a straightforward procedure. The treatment strategy often involves multiple embolization sessions, as the aneurysm may recanalize or show residual filling after initial interventions. This phenomenon, sometimes described as the water hammer effect, signals a sudden, pulsatile backward flow that can indicate the need for further treatment.
For clinicians, each embolization session offers both a technical challenge and an opportunity to fine-tune the approach. The procedure involves:
- Securing access via a suitable artery (e.g., the right axillary or femoral artery).
- Deploying a stent to protect essential branches supplying the liver and other organs.
- Using detachable embolization coils of various sizes to fully occlude the aneurysmal sac.
- Monitoring intra-procedural blood flow to ensure that the aneurysm is excluded from arterial circulation.
Each of these steps involves its own little details that require careful planning. What might seem like a standard endovascular procedure can quickly become a nerve-racking endeavor when the unique anatomical features of MALS and collateral flow are factored in. In this context, the need for a staged approach is evident. However, even with multiple sessions, the possibility of recanalization remains a tangible risk—a stark reminder of the persistent challenges in treating these lesions.
Furthermore, the use of embolization materials introduces additional loaded issues. Artifacts from previous procedures can hinder follow-up imaging and cloud the clinician’s judgment on when further intervention is warranted. This need for re-intervention, combined with the patient’s ongoing reluctance for surgery, reiterates the fact that managing these cases is as much an art as it is a science.
Taking a Closer Look at Imaging Modalities and Their Limitations
While endovascular therapy continues to evolve, imaging remains a cornerstone of both diagnosis and follow-up monitoring. The benefits of computed tomography angiography (CTA) are well recognized in providing detailed views of vascular anatomy. However, when reinforced by previous implants or embolic materials, CTA can present images that are difficult to interpret. This scenario compels clinicians to dig into alternative imaging strategies and sometimes even combine modalities to overcome the obstacles.
For instance, Doppler ultrasound—though highly operator-dependent—can be employed as a supplementary tool when CTA images are compromised. In such cases, having a multimodal imaging strategy is critical. Below is a bullet list highlighting the approaches used:
- CTA: Offers high-resolution images but is susceptible to artifacts (especially from metal implants).
- Doppler Ultrasound: Provides real-time flow information, though its clarity depends on the operator’s skill.
- Contrast-Enhanced Imaging: Can sometimes be used to better delineate vascular structures, yet it too may be hindered by interference from previously placed devices.
- Advanced Reconstruction Algorithms: Emerging software that minimizes artifact distortion and aids in 3D visualization is becoming increasingly vital.
Addressing these small distinctions in imaging techniques is key to improving patient outcomes. The reliance on imaging means that any shortfall in clarity can directly impact clinical decision-making. Therefore, it becomes critical to explore not only the available options but also potential innovations that could help mitigate these issues in future cases.
Optimizing Treatment Approaches: Shared Decisions and Clinical Adaptability
One of the strong takeaways from the case at hand is the importance of individualized, patient-centered care. When the patient opts out of surgical intervention, the medical team is left to find their way through a series of less invasive maneuvers. This process is full of problems and requires both clinicians and patients to be in constant dialogue as the condition evolves.
Adapting treatment strategies to account for both the technical challenges and the patient’s evolving condition is critical. In the face of recanalization or continued aneurysm growth, the following points become super important for future management:
- Multidisciplinary Approach: Collaboration among vascular surgeons, interventional radiologists, and imaging specialists is key to crafting a nuanced treatment plan.
- Comprehensive Follow-Up: Meticulous tracking of aneurysm size and blood flow using a combination of imaging modalities ensures that any subtle signs of recurrence are promptly addressed.
- Patient Education: Helping patients understand the rationale behind each step, including the potential need for multiple interventions, builds trust and facilitates shared decision-making.
- Flexibility in Management: The treatment protocol must be adaptable, ready to shift gears should the clinical situation change or if new imaging technologies become available.
This adaptive mindset is essential because every case of MALS with accompanying SMA aneurysm presents its own set of hidden complexities. The blend of evolving vascular dynamics, imaging challenges, and patient preferences creates a scenario where the treatment plan must remain dynamic and responsive.
The Role of Emerging Technologies in Overcoming Imaging Barriers
In recent times, innovations in imaging technology have offered hope in mitigating some of the problematic issues associated with artifact interference. New software algorithms designed for artifact reduction are beginning to show promise in helping radiologists and interventionalists get around the twisted issues brought on by metal implants and previous embolization materials.
For instance, advanced 3D reconstruction tools and contrast-enhanced techniques are gaining traction among professionals who demand as much precision as possible in their follow-up assessments. These evolving tools are not just technical niceties—they are key components that could reshape the way clinicians interpret follow-up imaging data and confirm the effectiveness of embolization procedures.
The table below highlights a few emerging technologies and their potential impacts:
| Technology | Potential Benefit |
|---|---|
| 3D Reconstruction Algorithms | Reduced artifact interference and enhanced visualization of aneurysm architecture |
| Contrast-Enhanced Ultrasound | Improved flow dynamics assessment despite the presence of metallic implants |
| Artifact Reduction Software | Better delineation of vascular structures in CTA imaging |
| Fusion Imaging Techniques | Combining data from different modalities to provide a comprehensive overview |
Clinicians must stay at the cutting edge of these innovations. As technology evolves, so too does the capacity to manage complicated vascular cases more effectively. It is essential to integrate these tools into clinical practice so that imaging—and by extension, treatment—can continue to improve. Such efforts might one day reduce the number of repeated interventions a patient must endure and improve long-term outcomes considerably.
Reflections on the Limitations of Current Endovascular Therapies
Even with the promising potential of endovascular therapy, the case discussed brings to light some enduring challenges. Repeated embolization procedures, while minimally invasive, have not entirely conquered the problem of aneurysm recurrence. Residual contrast filling and the gradual re-expansion of the aneurysm sac, despite multiple sessions, raise critical questions about the long-term effectiveness of available embolic materials and techniques.
These challenging bits of treatment underline that even the most refined endovascular approaches have limits when confronted with unusual vascular configurations and persistent collateral circulation. The following points summarize these limitations:
- Recanalization Risk: Even with successful initial embolization, the risk of blood flow returning to the aneurysm can necessitate further intervention.
- Material Limitations: The current generation of embolization coils, while effective, may not always guarantee complete occlusion in anatomically complex cases.
- Technical Demand: Multiple staged procedures require significant expertise and can be physically and emotionally overwhelming for both patient and practitioner.
- Imaging Dependence: The success of the therapy is heavily reliant on follow-up imaging that, as mentioned earlier, may be compromised by artifacts.
Each of these points emphasizes the need for continued research and development. Clinicians must be open to both learning from existing case experiences and integrating future innovations that could bridge these existing gaps. While endovascular therapy has revolutionized the approach to vascular aneurysms, it remains clear that prolonged management in cases complicated by MALS is a journey riddled with tension and requires constant vigilance.
Exploring Future Directions and Patient-Centered Outcomes
Looking forward, it is evident that there is a pressing need to improve protocols for the management of visceral artery aneurysms in patients with MALS. Future research may be aimed at refining embolization materials, developing better imaging techniques, and creating a more robust framework for deciding when surgical options should be considered despite patient hesitation.
Several research pathways and strategic improvements appear promising:
- Material Science Innovations: Development of next-generation embolic materials that offer a more durable occlusion and reduce the likelihood of recanalization.
- Integrative Imaging Platforms: Combining multiple imaging modalities with cutting-edge algorithms to mitigate the confusing bits caused by artifacts and provide a clearer view of the aneurysm’s status.
- Clinical Trials and Registries: Establishing multicenter studies to evaluate long-term outcomes of endovascular therapy in MALS patients can help standardize treatment protocols that are currently based on isolated case experiences.
- Enhanced Patient Communication: Tools that help patients understand the risks, benefits, and potential uncertainties in treatment can support shared decision-making and ultimately lead to better adherence to follow-up plans.
It is worth noting that as clinicians and researchers work together, the improvement in treatment modalities must always be balanced with a sensitivity to patient choices. In cases where surgery is declined, the evolution of endovascular techniques, along with better imaging and materials, will be essential in managing these high-risk scenarios.
We must also take a closer look at patient-reported outcomes and quality of life measures. The ultimate goal is not just to achieve a technically successful embolization, but to ensure that patients experience minimal discomfort and a high quality of life over the long run. Their experiences provide essential feedback that can help refine treatment strategies and make the entire process less intimidating for future patients.
Conclusion: Balancing Innovative Endovascular Techniques with Patient Realities
Managing large SMA aneurysms secondary to MALS is a journey filled with twisted parts, subtle details, and a constant need to balance technical precision with patient preferences. The case presented reminds us of the importance of utilizing a multidisciplinary approach, embracing emerging technologies, and fostering transparent communication with patients who must make difficult choices about their care.
In many ways, the story of this patient encapsulates the broader challenges facing modern vascular care. Despite the nerve-racking potential of repeated interventions and imaging hurdles, the evolution of endovascular therapy has opened up pathways that were once considered too intimidating to traverse. However, as we move forward, it is clear that further research, innovation, and adaptive protocols are super important for better long-term outcomes.
As clinicians work through these tangled issues, the dual emphasis must always be on technical excellence and holistic care. Only by addressing both the hidden complexities of vascular anatomy and the emotional and physical needs of the patient can we hope to build a truly effective treatment paradigm for MALS-related aneurysms. The dialogue between patient and provider remains at the heart of this journey, ensuring that every step reflects both scientific innovation and compassionate care.
In summary, while endovascular embolization has proven to be a powerful tool in the management of challenging aneurysms, its repeated use in cases riddled with recanalization and imaging limitations underscores the ongoing need for advancement. Every twist and turn in the treatment path carries lessons that can eventually lead to more robust and durable outcomes. With sustained efforts from researchers, clinicians, and medical technologists, the future holds promise for overcoming these challenges, thereby ensuring that patients receive care that is not only minimally invasive but also reliably effective.
By taking a thoughtful and multi-pronged approach, the field can build on its success stories and continuously improve strategies to manage vascular conditions marked by complex collateral circulation. This journey—full of both achievements and setbacks—serves as a reminder that excellence in healthcare is a dynamic process, one where every small improvement can lead to a significant enhancement in patient quality of life.
The experience of managing a large SMA aneurysm in the context of MALS forces us to confront both the technical challenges of embolization and the larger, patient-centered issues that underlie every treatment choice. As we continue to push the envelope on innovation and patient care, let us remain committed to finding our way through the tricky parts, the tangled issues, and the intimidating choices that define modern vascular medicine.
Read more about this topic at
Endovascular Management of Complex Aortic Aneurysms …
Endovascular repair of complex aortic aneurysms

