Subretinal Drusenoid Deposits and Their Impact on Age-Related Macular Degeneration
Recent findings have brought to light some interesting observations regarding subretinal drusenoid deposits (SDDs) in patients with age-related macular degeneration (AMD). In particular, data from a study conducted at the New York Eye and Ear Infirmary of Mount Sinai have revealed that SDDs in Black and Hispanic patients with AMD may signal a heightened risk for vascular diseases. As an editor deeply invested in the quality, nuance, and practicality of healthcare news, I invite you to take a closer look at these developments and consider how they might influence our future approaches to screening, diagnosis, and patient management.
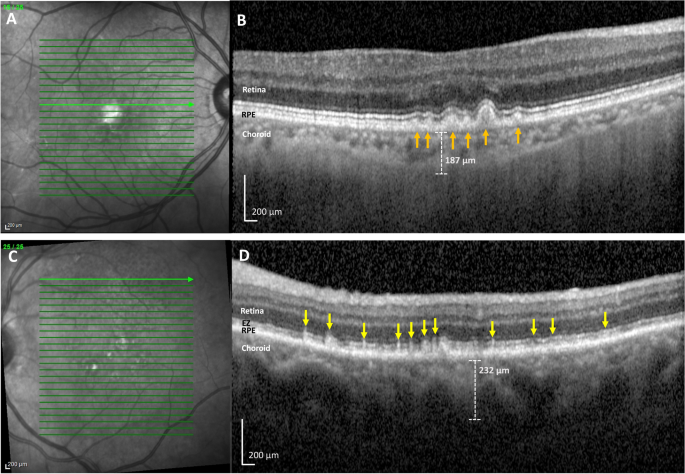
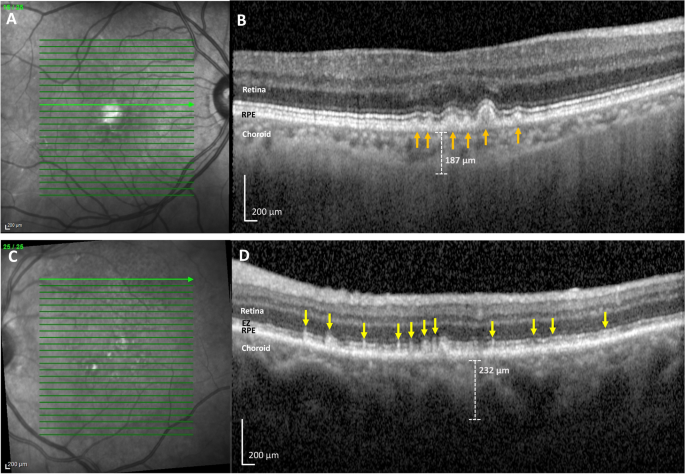
It is important to note that SDDs represent one of the two main forms of intermediate AMD evident on optical coherence tomography (OCT) images, the other being soft drusen. However, it appears that SDDs have particular implications in terms of disease progression and the risk of vascular complications. This poses not only a clinical puzzle but also a call to reexamine our methods and protocols for evaluating patients from diverse backgrounds.
Exploring the Link Between AMD and Vascular Diseases in Minority Populations
The recent study has shown that SDDs, when present in Black and Hispanic patients with AMD, might be associated with a higher likelihood of cardiovascular events such as myocardial infarction, congestive heart failure, and strokes. In essence, these deposits seem to mark patients who are at a greater overall risk for vascular diseases, much like what has been observed among White patients with AMD. Although there were no noticeable phenotypic differences in the presentation of SDDs between these racial groups, the implications for patient care are significant.
To illustrate the importance of these results, consider the following bullet list, which summarizes the evidence gathered:
- SDDs are closely linked with more rapid progression of AMD compared to soft drusen.
- Patients with SDDs tend to have thinner choroids, a finding confirmed by OCT imaging.
- Lower high-density lipoprotein (HDL) levels have been observed in patients presenting with these deposits.
- The presence of SDDs has been statistically associated with a higher risk of vascular conditions in all studied groups.
These findings underline the need to shift our focus from merely categorizing AMD based on the type of drusen present to considering the overall health risks, particularly vascular complications, that these patients face.
Detailed Insights into Optical Coherence Tomography Findings
Optical coherence tomography (OCT) is a crucial imaging tool that allows clinicians to “get into” the finer details of AMD pathology. Through OCT, physicians can distinguish between soft drusen and SDDs, even when the differences might seem subtle. Unfortunately, the process of differentiating these features is often tangled with tricky parts and confusing bits, making a robust understanding essential for delivering the best possible patient care.
A closer look at the OCT findings reveals that:
- SDDs usually present as distinctive deposits located in the subretinal space, clearly distinguishable from the soft drusen found within the retinal pigment epithelium.
- Patients diagnosed with SDDs tend to have thinner subfoveal choroidal layers—a factor that is frequently linked to a worse prognosis.
- The detailed imaging provided by OCT is not only critical for diagnosis but also for monitoring disease progression, thereby enabling timely intervention before complications become overwhelming.
For clinicians, the advantage of OCT is that it allows them to figure a path through the maze of AMD complexities while ensuring that no subtle details remain unnoticed. Experts are now calling for a more comprehensive approach that integrates these imaging findings with systemic health evaluations.
Screening and Early Intervention: Addressing the Tangled Issues
The significance of these discoveries underscores how essential it is to embark on rigorous screening protocols, especially for minority populations who are at a disproportionate risk for vascular diseases. A diligent search for SDDs in Black and Hispanic patients with AMD is not merely advisable; it is key to uncovering additional health risks that may otherwise go unnoticed.
Early detection can be daunting for both patients and clinicians alike. However, by applying a multi-faceted approach that includes:
- Regular OCT imaging for early identification of SDDs
- Routine cardiovascular and lipid profile screenings
- Customized patient education on the risks associated with both AMD and vascular diseases
healthcare professionals can more effectively steer through both ocular and systemic complications. Although the idea of such comprehensive screening might seem overwhelming initially, the potential benefits—namely, reducing the risk of both vision loss and heart-related events—far outweigh the challenges.
Interpreting the Nitty-Gritty of Choroidal Thickness and HDL Levels
One of the more intriguing aspects of the study is the association between SDDs and both choroidal thickness and HDL levels. With patients showing a consistently thinner choroid and lower HDL levels, it becomes important for clinicians to not just focus on ocular findings but also consider the broader implications for cardiovascular health.
Let’s break down these findings in a clear and organized table:
| Parameter | Findings in Patients with SDDs | Findings in Patients without SDDs |
|---|---|---|
| Subfoveal Choroidal Thickness | Approximately 166.6 ± 59.2 µm | Approximately 208.5 ± 83.2 µm |
| HDL Levels | Approximately 52.4 ± 11.7 mg/dL | Approximately 60.2 ± 15.6 mg/dL |
These numbers not only emphasize the subtle differences present in the ocular structure but also serve as a reminder of the interconnectedness of various parts of the body. Lower HDL levels, often referred to as “good cholesterol,” combined with a thinner choroid, may hint at a systemic issue that could predispose patients to cardiovascular problems.
Reconciling Modern Medicine with Alternative Approaches
While research in modern medicine has provided us with these critical insights, there is also an emerging interest in how alternative approaches can complement conventional therapies. A holistic evaluation of patient health can sometimes benefit from integrating alternative medicine practices alongside modern diagnostic tools like OCT.
For example, nutrition and lifestyle modifications have a key role in managing both AMD progression and cardiovascular risk. Patients may experience improvements in their lipid profiles and overall vascular health through:
- Adopting a diet rich in omega-3 fatty acids and antioxidants
- Regular physical activity tailored to their ability
- Stress-reduction techniques such as meditation or yoga
These interventions, while not replacing conventional therapy, can help dig into some of the root causes of disease progression and add another layer to our management strategies. By bringing modern medicine together with alternative practices, healthcare providers can offer a more balanced and individualized approach that doesn’t ignore the fine points of patient care.
Managing Your Way Through Study Findings: The Clinical Perspective
From the clinician’s point of view, this study leaves us with a series of important practical questions. How do we adjust our screening protocols to better identify SDDs in minority patients? What does this mean for the management of AMD in today’s multifaceted healthcare environment? The answers lie in working through the findings and ensuring that no stone is left unturned.
Practitioners are encouraged to incorporate the following measures into their daily routines:
- Enhanced imaging techniques to better capture the subtle details of drusen formations
- Regular monitoring of lipid profiles and cardiovascular parameters
- Cross-disciplinary collaboration between ophthalmologists and cardiologists
- Patient education sessions that explain the connection between eye health and overall vascular risk
Taking these actions not only helps in managing the tricky parts of patient evaluation but also builds a bridge between ocular health and broader systemic concerns. The integration of these strategies is not a one-size-fits-all approach; it requires a thoughtful application tailored to each patient’s unique presentation and health history.
Exploring the Broader Implications for Clinical Practices
It is not uncommon for studies like these to prompt a reevaluation of our current methodologies. In many ways, the evidence provided by the study acts as an impetus for a more integrated, multidisciplinary approach to patient care. The strong association between SDDs and vascular diseases in Black and Hispanic patients with AMD should encourage clinicians to take an inclusive view of disease management—one that goes beyond the eye and considers the heart and blood vessels, too.
This research reminds us that conditions such as AMD cannot be isolated from the rest of the body. Instead, they should be understood as part of a broader health picture that involves multiple systems interacting in subtle, yet important ways. For instance, the presence of SDDs may serve as a red flag that should trigger a more thorough examination of cardiovascular health in any patient, regardless of race.
It is both a challenge and an opportunity for healthcare professionals. The challenge lies in deciphering the tangled issues associated with early diagnosis and rapid intervention. The opportunity, however, is in setting up a paradigm that is proactive rather than reactive. Not only does this improve patient outcomes, but it also emphasizes the need for coordinated care that addresses both ocular and systemic issues.
Fine Points of Integrating Research into Practice
In order to make the best use of emerging research, practitioners must be willing to get into the nitty-gritty of each case. No longer can we view AMD in isolation from other health risks. Instead, clinicians must take a comprehensive view, recognizing the following key aspects:
- Timely Diagnosis: Early recognition of SDDs via OCT imaging is super important. This helps in predicting not only the visual prognosis but also potential systemic complications.
- Risk Stratification: By evaluating both ocular findings and systemic indicators (such as HDL levels), providers can build a more accurate risk profile for each patient.
- Multidisciplinary Collaboration: Seamless communication between the eye care team and primary care or cardiovascular specialists is critical in administering holistic care.
- Patient Engagement: Informing patients about the potential connections between their eye health and overall cardiovascular risk empowers them to take control of their well-being.
Such integrated care not only benefits patients in the short term by providing targeted interventions but also contributes to long-term health outcomes. The collaboration between different specialties can help soothe some of the overwhelming challenges that both patients and providers face when dealing with complex conditions.
Figure a Path Forward: Implications for Future Research and Policy
With studies like this paving the way, there is genuine optimism regarding the transformation of clinical practices and healthcare policies. Future research needs to continue exploring these subtle links between ocular pathologies and systemic diseases. The hope is that continual investigation will lead to therapies that are not only more effective but also personalized to the needs of a diverse population.
Policymakers and healthcare administrators must also take note of these insights and work toward creating environments where early screening and integrated care are the norm rather than the exception. This might involve:
- Allocating more resources for advanced imaging equipment in community clinics
- Establishing guidelines that encourage comprehensive cardiovascular evaluations for patients diagnosed with AMD
- Promoting educational programs that help both providers and patients recognize the early signs of systemic disease linked to ocular changes
By implementing these measures, the healthcare system can better steer through the tricky parts and make informed decisions that benefit everyone, especially those in high-risk groups.
Taking a Closer Look at the Patient Experience
As we consider the clinical and policy implications, we must also remember the direct impact on patient lives. For many patients, receiving a diagnosis of AMD, combined with the knowledge of potential vascular risks, can be nerve-racking. However, a transparent and empathetic approach to care can make a huge difference.
Patients should be educated on the following key areas:
- What SDDs are and why they matter
- How AMD and vascular health are interrelated
- Simple lifestyle changes that can help improve overall health
- The importance of regular screening and active participation in one’s own care
This patient-centered approach can also help to demystify the confusing bits of medical terminology and diagnostic jargon. When patients understand the nature of their conditions and the rationale behind various tests and interventions, they are better equipped to comply with treatment and make informed decisions about their health.
Working Through the Small Distinctions in Risk Assessment
One of the challenges in the current landscape is to make sense of the little twists and subtle details that differentiate one case from another. For instance, while the overall prevalence of SDDs in Black and Hispanic patients appears similar to that in White patients, the associated risks and outcomes may differ in ways that require a tailored approach to each patient’s care.
Healthcare practitioners can benefit from adopting a systematic risk assessment strategy that includes:
- Detailed ocular imaging reviews
- Comprehensive blood lipid profiling
- Consideration of the patient’s overall cardiovascular risk
- Regular follow-up appointments to monitor changes in both eye and vascular health
By breaking down patient data into manageable components, clinicians can overcome the tangled issues that come with multi-system diseases and provide care that is truly responsive to the individual’s needs.
Finding Your Path in an Evolving Healthcare Landscape
The integration of these robust research findings into everyday practice is a journey filled with twists and turns. However, there is no doubt that such integration is essential to enhancing the quality of care that patients receive. By embracing a fully integrated approach—one that connects advanced imaging techniques, comprehensive risk assessments, and effective patient communication—healthcare professionals can drive forward a new era of precision medicine.
This evolution is likely to be on edge with both challenges and opportunities. Yet through dedicated collaboration among specialists, persistent efforts in research, and a commitment to patient well-being, we can figure a clear path forward that benefits all parties involved.
Conclusion: Connecting the Dots Between Eye Health and Systemic Well-Being
In summary, the study highlighting the presence of SDDs in Black and Hispanic patients with AMD raises several critical issues for patient evaluation and care. By drawing connections between ocular findings and systemic conditions, the research underscores the necessity of using comprehensive, multidisciplinary strategies to manage these intertwined health risks.
From the finer details of OCT imaging to the broader implications for cardiovascular health, this research invites all stakeholders—clinicians, researchers, policymakers, and patients—to get into the discussion and reexamine how we approach both AMD and vascular diseases. The ultimate goal is to ensure that every patient, regardless of background, receives a level of care that is as balanced, proactive, and comprehensive as possible.
It is my belief, as an editor committed to clarity and the practical application of medical research, that we must learn from these findings. By working through the small distinctions and tricky parts with open minds and collaborative efforts, we can bring about positive changes that benefit our communities at large. Let this study be a reminder that our responsibility extends beyond treating a single symptom—instead, it challenges us to bridge the gaps between various aspects of health, creating a future where precision medicine and integrated care are not just ideals, but everyday realities.
Originally Post From https://www.ophthalmologytimes.com/view/subretinal-drusenoid-deposits-in-black-and-hispanic-patients-with-amd
Read more about this topic at
How to Manage Deposit Risk in the Modern Age
Protecting Banks from Credit & Deposit Concentration Risk