Examining Genicular Artery Embolization for Knee Osteoarthritis: A Fresh Perspective
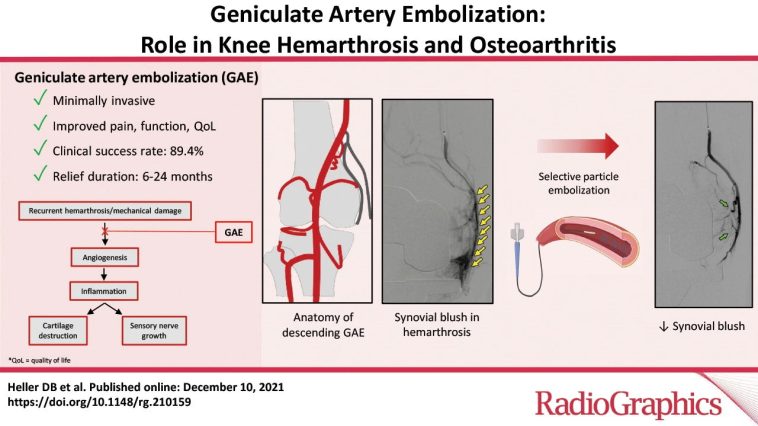
Recent advances in minimally-invasive treatments have led clinicians and patients alike to take a closer look at genicular artery embolization (GAE) as a promising method for managing symptomatic knee osteoarthritis (KOA). Recent studies, such as the one published in the Journal of Vascular and Interventional Radiology, report that GAE not only relieves pain but might also slow the progression of osteoarthritis by reducing specific biomarker levels. In this opinion editorial, we explore the background, techniques, clinical outcomes, and the possible future of GAE by digging into the study details and the broader context of knee OA management.
As we examine the research, it is important to note that this new procedure is being considered alongside traditional treatments. Although many find the idea of arterial embolization intimidating at first, the results so far have been promising. With new studies demonstrating significant improvement in patient-reported pain outcomes, GAE is emerging as a potential alternative for those with troublesome knee pain.
Understanding Genicular Artery Embolization as a Treatment Option
Genicular artery embolization is a procedure that involves the targeted blocking of small blood vessels that supply areas of the knee joint associated with inflammation and pain. Using tiny microspheres (250-µm in the study), interventional radiologists guide a catheter to the problematic arteries and release the embolic material, thereby reducing the blood flow that may be feeding the irritating areas.
This approach represents a marked shift from traditional methods, which typically rely on medications, physical therapy, and even surgical interventions. GAE provides patients a minimally-invasive option that might lessen the need for more extensive procedures while offering relief from chronic knee pain.
Key Differences Between Traditional Treatments and GAE
While knee osteoarthritis has long been managed through conventional treatments – such as nonsteroidal anti-inflammatory drugs, corticosteroid injections, and even total knee replacement in severe cases – GAE introduces a novel pathway. It works by targeting the subtle parts of the underlying inflammatory process in the joint, potentially curbing both pain and disease progression.
This innovative technique offers a different perspective on OA management and appeals to patients who have encountered several tangled issues with traditional care approaches, including the limited duration of pain relief and the nerve-racking recovery times associated with surgery.
Analyzing the Study’s Methods and Outcomes
In the referenced study, 25 patients with symptomatic KOA that had not responded to at least three months of conservative management underwent GAE. The technical success rate was 100 percent – a testament to the precision and reliability of the method – and there were no significant adverse events. The clinical success rate, defined by a meaningful reduction in pain, exceeded 60 percent within the patient population.
Patient-reported outcome measures, which are critical when evaluating new therapy, were taken at baseline and at successive intervals: one, three, and 12 months post-procedure. These measures included the visual analog scale (VAS) pain scores and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores, providing a composite view of pain, stiffness, and function.
Technical Success and Patient Safety
One of the crucial takeaways from the study is the impeccable technical success, as evidenced by a 100 percent rate in the execution of the procedure. Such results indicate that when performed by skilled interventional radiologists, GAE can be carried out safely with only minimal challenges – the kind of tricky parts and tangled issues that are inherent in any medical procedure.
This high level of safety is particularly important for patients who have been dealing with off-putting side effects from medications and the intimidating possibility of open surgery. GAE offers a less invasive option that still manages to deliver significant clinical benefits without the nerve-racking complications that sometimes accompany more aggressive interventions.
Patient-Reported Outcomes: A Closer Look at Pain Reduction
The study revealed impressive reductions in pain, with VAS scores decreasing by approximately 48.5 percent at one month, 50.8 percent at three months, and 55.4 percent at 12 months. These figures do more than just highlight the procedure’s potential in easing pain; they suggest that the effects of GAE become more pronounced over time.
Similarly, the WOMAC scores, which focus on the overall impact of osteoarthritis on daily activities, also showed significant improvement, with reductions of around 39.6 percent at one month, climbing to 50.1 percent at three months before slightly receding to 43.7 percent at the 12-month mark. Such numbers provide a reassuring picture for patients who are dealing with the overwhelming burden of persistent knee pain.
Biomarker Findings and Their Implications
A noteworthy aspect of the study was the observation of changes in biomarkers following GAE. At 12 months, there was a significant decrease in vascular endothelial growth factor (VEGF) and the interleukin-1 receptor antagonist (IL-1Ra). These signaling proteins are believed to play a role in the inflammatory process that drives osteoarthritis progression.
The decrease in VEGF, which stimulates the formation of new blood vessels, could point to a reduced capacity for the body to fuel the inflammatory parts of the knee joint. Similarly, a fall in IL-1Ra levels may suggest a modulation of the local inflammatory response over time. Although no significant shifts were observed in other biomarkers, these particular findings add another layer to our understanding, suggesting that GAE might not only relieve symptoms but also influence the underlying disease process.
Understanding the Subtleties of Pain Relief Through GAE
The reported patient outcomes provide insight into both the immediate and sustained benefits of GAE. Pain reduction is not merely a by-product of numbness or temporary relief; it appears to also involve a shift in the inflammatory environment within the knee joint. For many who have waded through the nerve-racking journey of traditional therapies, the promise of a treatment that might provide ongoing relief – even if modestly so – is galvanizing.
While the study is limited by the small sample size of 25 patients, it nevertheless sheds light on the subtle details of the procedure’s effectiveness. The reduction in pain scores over time suggests that continuous improvement is possible and that GAE might offer a super important alternative for patients whose treatment options have become too tangled and frustrating.
The Role of Patient-Reported Outcomes in Assessing GAE
Patient-reported outcomes are critical when assessing the success of any new treatment, especially one that deals with pain management. Tools such as VAS and WOMAC scores enable physicians to get into the nitty-gritty of how the procedure affects a patient’s day-to-day life. These measures are easily relatable and provide clear, numerical evidence of the benefits experienced.
For those suffering from chronic knee pain, the ability to report lower pain levels and improved functionality is essential. This means that even as the procedure might appear intimidating at first glance, the outcome in terms of enhancing quality of life can be a deciding factor for many individuals.
Evaluating the Benefits of GAE in Knee Osteoarthritis Management
As we compare GAE to the standard care options available for knee osteoarthritis, several key benefits emerge:
- Minimally-Invasive Approach: GAE is performed via a catheter-based procedure, avoiding the longer recovery times and risks associated with open surgery.
- Rapid Pain Relief: With significant reductions in pain observed as early as one month post-procedure, patients can experience rapid improvements.
- Potential Disease-Modifying Effects: The noted changes in biomarkers like VEGF suggest that GAE may influence the inflammatory drivers of osteoarthritis over time.
- High Safety Profile: The study reports no significant adverse events, making it a relatively low-risk option for patients who have already faced the intimidating prospects of traditional surgeries.
These benefits position GAE as a super important addition to the treatment armamentarium for KOA, offering hope for those who have seen limited success with other interventions.
Tabulated Summary of Patient Outcomes and Biomarkers
| Outcome | 1 Month | 3 Months | 12 Months |
|---|---|---|---|
| VAS Pain Score Reduction (%) | 48.5% | 50.8% | 55.4% |
| WOMAC Pain Score Improvement (%) | 39.6% | 50.1% | 43.7% |
| VEGF Levels | Not significantly changed | Not significantly changed | Significantly decreased |
| IL-1Ra Levels | Not significantly changed | Not significantly changed | Significantly decreased |
This table offers a quick snapshot of the clinical benefits observed and underscores the persistent improvements in pain metrics, which are especially important for anyone looking into alternatives amid the confusing bits of knee osteoarthritis management.
Weighing the Clinical Evidence: The Good, the Tricky, and the Overwhelming
The clinical evidence so far paints a promising picture for GAE. However, every treatment modality has its tricky parts and challenges, and GAE is no exception. Consider the following:
- Limited Sample Size: The initial studies have involved small patient cohorts, which means that while the early results look promising, larger trials are necessary to confirm these findings.
- Procedure Standardization: As with any emerging technique, variations in how the procedure is performed across different centers can lead to slightly different outcomes.
- Long-Term Effectiveness: The long-term benefits beyond one year remain to be fully established, and patients may need to cope with further tweaks or repeated procedures over time.
- Patient Selection: Not everyone with knee osteoarthritis is a suitable candidate. Determining which patients might achieve the best outcomes with GAE requires further research.
Due to these mixed factors, clinicians must remain cautious and balanced when reviewing the available evidence. It is critical to figure a path through the fine points of the data, using a combination of patient history, clinical judgment, and evolving research trends.
Deciphering the Impact on Quality of Life
One of the most compelling aspects of GAE is its potential to enhance everyday life for patients who have long struggled with debilitating knee pain. Chronic OA pain can disrupt sleep, limit mobility, and even dampen emotional well-being. It is essential that treatments aim not only for numerical improvements but also real-world benefits.
By seeing statistically significant declines in pain scores and experiencing fewer complications compared to surgical alternatives, patients can enjoy improved quality of life. This is especially important for those who have been through the overwhelming maze of conventional therapies without adequate relief.
Comparing GAE With Other Minimally-Invasive Procedures
GAE stands distinct from other commonly employed minimally-invasive interventions for knee osteoarthritis. While options like viscosupplementation and radiofrequency ablation are also used, GAE distinguishes itself by targeting the little details of the blood flow to the joint, thereby potentially reducing inflammation from its roots.
A comparative look at these treatments reveals:
- Viscosupplementation: Focuses primarily on lubricating the joint but may not address underlying inflammation adequately.
- Radiofrequency Ablation: Targets nerve signaling to manage pain but does not usually alter the disease process itself.
- GAE: Offers the possibility of intervening in the inflammatory cascade by reducing blood vessel activity, which can result in both immediate and sustained pain relief.
Making your way through these options depends on individual patient profiles and preferences. It is key for patients and clinicians to discuss the potential benefits and limitations of each treatment, ensuring that decisions are as informed as possible.
The Patient Perspective: What to Expect from GAE
From the patient viewpoint, it is important to understand the step-by-step journey involved with GAE:
- Consultation and Evaluation: A thorough review of the patient’s medical history and imaging studies is the first step. This helps determine whether GAE is a suitable method to address the specific pain points in the knee.
- The Procedure: Conducted by interventional radiologists with a high level of expertise, the process involves a simple catheter-based approach that is generally done on an outpatient basis.
- Recovery and Follow-Up: Post-procedure follow-up includes monitoring for any immediate adverse events and assessing pain levels at intervals, ensuring that improvements are sustained over the long haul.
Patients are encouraged to ask questions, understand the potential side effects, and weigh the pros and cons of GAE compared to other minimally-invasive procedures. Being proactive about one’s healthcare can help steer through the maze of treatment options available.
Anticipated Challenges and the Need for Larger Studies
The early results of GAE are promising, yet they also raise several questions that warrant further exploration. For instance, the small sample size of the initial studies makes it difficult to generalize the outcomes. Additionally, while the decrease in certain biomarkers is an interesting finding, more research is needed to firmly establish the link between these changes and long-term osteoarthritis progression.
It is essential that larger, randomized controlled trials are conducted to validate the preliminary findings and to address the following concerns:
- How does GAE compare directly with other standard treatments? A head-to-head comparison in a large patient cohort would clarify potential advantages.
- What is the optimal patient profile? Refining criteria for patient selection will help ensure that those most likely to benefit are identified early in the treatment process.
- What are the long-term effects? Monitoring patients over several years will provide insights into whether the benefits of GAE remain consistent or require adjustments over time.
Addressing these points in future studies will contribute to a more robust understanding of the procedure and help clinicians figure a path through the subtle details of patient management.
Future Directions for Minimally-Invasive Knee Osteoarthritis Treatments
As research into genicular artery embolization and related techniques continues, several avenues for future inquiry are emerging. Medical professionals and researchers are increasingly interested in understanding not only the symptomatic relief that procedures like GAE provide but also whether they can alter the long-term course of osteoarthritis.
Potential future research directions include:
- Combination Therapies: Investigating whether GAE can be combined with other treatments such as physical therapy, weight management, or pharmacological interventions to provide comprehensive care.
- Biomarker Monitoring: Continuing to track changes in inflammatory markers to determine if these shifts can predict long-term clinical outcomes.
- Cost-Effectiveness Analyses: Comparing the overall costs of GAE relative to traditional methods may help establish its value within the healthcare system.
- Patient Satisfaction Studies: Beyond quantitative outcomes, understanding patient satisfaction can guide refinements in both technique and aftercare.
As these research areas are explored, the promise of a more tailored, patient-centric approach to knee osteoarthritis management grows even bolder. It is a future where minimally-invasive techniques might not only soothe pain but also address some of the root causes of joint degeneration.
Integrating New Insights with Clinical Practice
The potential benefits of genicular artery embolization have sparked a wave of optimism in the medical community. However, translating research outcomes into everyday clinical practice is often a process wracked with its own share of twists and turns. Clinicians need to combine rigorous scientific evidence with practical, patient-focused considerations.
To make the most of this emerging technique, healthcare providers might consider:
- Staying abreast of new research: Continuous education and review of emerging data are essential to integrate new techniques into clinical care effectively.
- Collaborating across specialties: Working with interventional radiologists, orthopedic surgeons, and rheumatologists can help optimize treatment pathways for patients.
- Patient education and informed consent: Providing clear, accessible explanations regarding how GAE works and what to expect can ease the anxiety often associated with innovative treatments.
- Tailoring treatment plans: As with all medical interventions, one size does not fit all. It is crucial to match the specific needs of each patient with the right therapeutic approach.
These steps are essential for integrating new treatment methodologies like GAE into the broader framework of knee osteoarthritis care, ensuring that the transition from research bench to the clinical bedside is as smooth as possible.
Conclusion: A Promising yet Cautious Outlook
To wrap up, genicular artery embolization offers an exciting potential in the landscape of knee osteoarthritis treatments. Its minimally-invasive nature, combined with the possibility of reducing inflammatory markers and providing substantial pain relief, positions it as a super important option for patients struggling with chronic KOA.
At the same time, the current evidence, while promising, remains limited by small sample sizes and short follow-up periods. As clinicians and researchers work together to iron out the tricky parts and address the hidden complexities, GAE might very well become a cornerstone in managing a condition that has long been weighed down by confusing bits of traditional therapy.
For patients and providers sorted out by the challenges of knee OA, this new approach offers not only a way to ease daily pain but also hope for a future where the progression of osteoarthritis itself could be slowed. The journey ahead is loaded with both promise and uncertainty, making continued research, open dialogue, and patient-centered care absolutely key.
In the end, the success of genicular artery embolization will be measured not only by reduced pain scores and improved mobility but also by how well it helps people navigate the often intimidating maze of osteoarthritis treatment. With further research and careful clinical application, GAE could become a game changer in the management of symptomatic knee osteoarthritis, potentially enhancing the quality of life for countless individuals.
As we take a closer look at the evolving world of minimally-invasive procedures, one thing remains clear: innovative treatments like GAE remind us that modern medicine is continually adapting to offer new solutions for age-old challenges. It is a journey that requires us to dig into the fine points of research, figure a path through the subtle details of patient care, and keep an open mind to methods that might transform how we manage chronic conditions in the future.
Ultimately, while the current evidence on genicular artery embolization is encouraging, further large-scale studies are needed to confirm its long-term effectiveness and delineate its role in the broader spectrum of knee osteoarthritis treatment. For now, GAE stands as a beacon of hope for patients who have been through the nerve-racking challenges of traditional treatments, offering a fresh outlook and a promising step forward in the complex world of chronic pain management.
With continued research and collaboration across specialties, the evolution of knee osteoarthritis treatment will likely reveal more about how best to integrate such innovative procedures into daily clinical practice. For healthcare providers and patients alike, staying informed and adaptable is the best way to ensure that progress in medical science translates into tangible benefits at the bedside.
In the rapidly advancing field of minimally-invasive treatments, genicular artery embolization is a compelling example of how modern medicine is embracing new ideas to tackle traditional problems. By focusing on the subtle details in the inflammatory process and providing sustained relief from pain, GAE not only offers hope for improved quality of life but also underscores the importance of innovation in healthcare. Only time will tell if this approach becomes a mainstay of KOA management, but the early data certainly encourage a cautiously optimistic outlook.
In conclusion, as we work through the challenging bits and fine shades of treatment options, genicular artery embolization emerges as a potentially transformative intervention. Its promise lies in the blend of technical precision, patient-centered outcomes, and the possibility of having a real and lasting impact on a condition that affects millions worldwide. For patients and clinicians seeking effective alternatives to traditional osteoarthritis management, GAE provides a pathway that is both intriguing and filled with hope.
Originally Post From https://www.endocrinologyadvisor.com/news/genicular-artery-embolization-safe-relieves-pain-for-symptomatic-knee-oa/
Read more about this topic at
Knee Pain: Causes & Treatment
Take control of your knee pain