Exploring a Rare Case of Rectal Vascular Malformation in Klippel-Trenaunay Syndrome
This opinion editorial takes a closer look at an unusual clinical case involving isolated colorectal vascular malformation in a patient with Klippel-Trenaunay Syndrome. In today’s evolving world of healthcare, cases like these offer deep insights into both the fine points of diagnostic approaches and the modern treatment choices available. I will be digging into the clinical details of the case, the challenges posed by this rare condition, and the various perspectives on managing it with the latest surgical and diagnostic tools.
The story revolves around a 45-year-old patient who experienced recurring pain, bleeding, and discomfort leading to a diagnosis that went far beyond ordinary hemorrhoidal issues. In many ways, this case embodies the tricky parts of modern medicine—untangling the confusing bits of symptoms that, at first glance, seem benign but eventually point to a rare vascular malformation.
Understanding the Syndrome and Its Uncommon Manifestations
Klippel-Trenaunay Syndrome is typically known for its three-part presentation: capillary malformations (often seen as port-wine stains), venous malformations, and limb overgrowth. However, this report highlights the isolated rectal involvement—a rare twist that many experts find both intriguing and challenging. Although abnormal vascular structures in the rectum are not typical of the syndrome, they underscore how a patient’s medical history can hide the more complicated pieces underneath a seemingly simple diagnosis.
How Is Rectal Vascular Malformation Diagnosed in Klippel-Trenaunay Syndrome?
For many clinicians, diagnosing rectal vascular malformations is like steering through a maze of subtle details and hidden complexities. Traditional symptoms such as perianal pain, recurring bleeding during defecation, and general weakness were seen in the patient, but these signs alone often lead to misinterpretation. In this case, colonoscopy initially indicated what appeared to be hemorrhoidal issues—a diagnosis that might have been considered straightforward if not for the unexpected imaging findings.
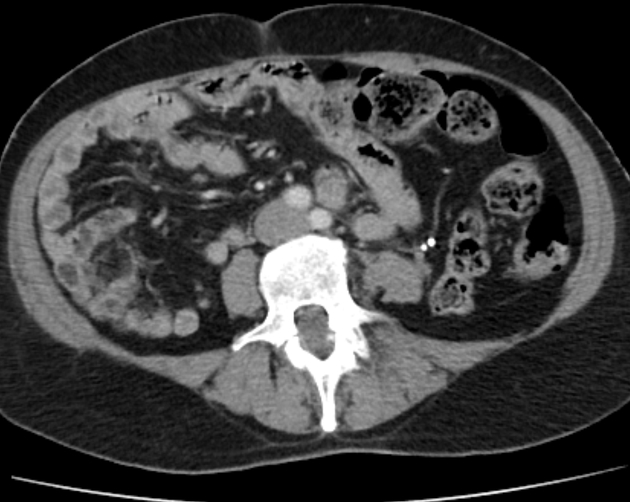
Modern technologies, such as multislice computed tomography (MSCT) combined with intravenous contrast, played a key role in unveiling the full picture. The use of this imaging technique helped expose not just an increased vascular pattern but also a large, irregular rectal lesion with uneven internal contours. These imaging findings triggered a deep investigation into whether the lesion was a mere hemangioma or something more complicated like a cancerous formation.
Below is a brief bullet list summarizing the diagnostic approach:
- Initial clinical evaluation: assessing pain, bleeding, and hemorrhoidal prolapse.
- Colonoscopy: exploring the extent of vascular involvement and noticing additional mucosal changes.
- MSCT with intravenous contrast: identifying the irregular shape, density variations, and signs of active blood perfusion in the lesion.
- Histopathological analysis: verifying the presence of vascular-type cavities, flattened endothelial linings, and thrombotic masses.
This systematic approach is essential in modern medicine because it helps doctors figure a path even when unexpected findings emerge. Such imaging and pathology data are critical in separating the needle from the haystack—ensuring that crucial details are neither overlooked nor misinterpreted.
The Role of Laparoscopic Surgery in Managing Complex Rectal Lesions
A major turning point in this case was the role of laparoscopic surgery, an option that is both innovative and less invasive compared to traditional open surgery. Many clinicians underscore the benefits of this approach because it minimizes trauma to the patient while allowing an in-depth look at the affected area.
In the highlighted case, the surgical team opted for a multistage strategy. This involved:
- First, implanting a temporary vena cava filter to mitigate the risk of pulmonary embolism from thrombosed varicose veins.
- Then, performing a laparoscopic-assisted anterior resection of the rectum with a preventive colostomy. This stage included a careful demucosation of the rectal lining to remove the diseased tissue.
- Finally, after ensuring proper recovery and stabilization, the closure of the colostomy was carried out.
The surgical approach was not only a means to treat the abnormal vascular lesion but also an essential diagnostic tool. Surgeons were able to inspect and verify the presence of large, blood-filled cavities in the resected tissue, confirming that the unusual lesion was indeed a form of vascular malformation rather than a common hemorrhoidal problem.
Digging into the Imaging Modalities: MSCT and Colonoscopy
One of the most notable aspects of this case is the interplay between different imaging techniques. The blend of colonoscopy and multislice computed tomography provided a comprehensive view of the vascular anomalies in the rectum. While colonoscopy mapped out the mucosal surface and identified areas of potential pathology, MSCT dove deeper into the submucosal layers.
A summary table below outlines the strengths of each imaging modality:
| Imaging Technique | Strengths | Challenges Addressed |
|---|---|---|
| Colonoscopy |
|
|
| MSCT with Intravenous Contrast |
|
|
Combining these methods allowed clinicians to piece together a much more detailed image of the lesion’s anatomy and vascular supply. The fact that the lesion was supplied by both pararectal and parametrial blood vessels pointed towards an abnormal angiomatous supply, which further confirmed the complexity of the condition.
Alternative Perspectives: When to Consider Conservative Versus Surgical Management
The road to reaching the optimal treatment option is rarely straightforward, especially when the clinical presentation is loaded with issues and the condition is as rare as rectal vascular malformation in Klippel-Trenaunay Syndrome. Some experts argue that conservative management could be an option if the patient is not experiencing severe symptoms or if the lesion is small and well-contained. However, in this scenario, repeated episodes of bleeding and the size of the malformation indicated that a radical approach was necessary.
Weighing the Options: Conservative Treatments and Their Limitations
Conservative treatments like sclerotherapy and ligation are often considered for more common vascular issues such as simple hemorrhoids. In the current case, however, the failure of standard methods to control the bleeding and to effectively treat the lesion made these methods off-putting choices. There is a notable risk that using conservative methods in such cases may merely postpone definitive care and potentially lead to severe complications.
Some of the common issues with conservative treatments in cases like these include:
- The potential for recurrent bleeding that is difficult to control.
- Incomplete resolution of the lesion, leaving residual vascular channels open and vulnerable.
- An increased risk of misdiagnosis or failure to recognize the full pathomorphological picture.
On the flip side, surgical intervention, especially through a minimally invasive lens like laparoscopy, offers a more direct method of excising the problematic tissue and mitigating the risk of future episodes. This case clearly demonstrates that when standard methods fall short, opting for a more radical approach can be not only necessary but also instrumental in preventing life-threatening complications.
Advantages of a Multistage Surgical Approach
The multistage surgical procedure chosen in this case had multiple benefits that went beyond simply removing the lesion. Staging the surgery allowed the medical team to manage the patient’s condition in manageable segments, significantly reducing the risk associated with one prolonged operation. The key advantages included:
- Reducing the probability of in-surgery complications, such as uncontrolled bleeding.
- Allowing ample time for proper patient recovery between stages.
- Providing enough time for detailed assessment of the patient’s response to each stage of treatment.
By first inserting a temporary vena cava filter, doctors effectively minimized the risk of pulmonary embolism—a life-threatening incident that could potentially arise from the thrombosed varicose veins. Following this, the laparoscopic resection not only provided relief from symptoms but also allowed the surgical team to obtain tissue specimens which proved key in confirming the diagnosis.
From Clinical Data to Opinion: What Can We Learn?
We face a scenario where modern imaging, careful pathology, and state-of-the-art surgical techniques come together to address an unusual presentation of vascular malformation. Here are some of the personal reflections and key takeaways based on the case presentation:
- Importance of Comprehensive Diagnostics: The combination of colonoscopy and MSCT proved to be an essential diagnostic duo, helping to untangle the twists and turns of a condition that might otherwise be misdiagnosed as simple chronic hemorrhoids.
- Timeliness of Intervention: The consequences of overlooking early warning signs could be overwhelming. Regular medical monitoring and prompt responses to recurring symptoms are super important for preventing complications.
- Modern Surgical Techniques Are a Game Changer: Laparoscopic surgery, as demonstrated, can offer a safer and more efficient means to both diagnose and treat this type of vascular malformation. Patients benefit not just from less recovery time but also from reduced surgical trauma and improved overall outcomes.
- Multidisciplinary Approach: Cases like these underline the need for specialists across the board—from radiologists to surgeons—working closely together to figure a path through complicated cases. This collaborative spirit plays a super important role in ensuring optimal patient care.
The story discussed above serves as a reminder that sometimes conditions which appear straightforward at first may hide a range of tangled issues beneath the surface. It encourages both patients and practitioners to take any sign of abnormality seriously and to consider a second opinion when standard treatments do not yield lasting relief.
Unraveling the Hidden Complexities Through Multidisciplinary Efforts
The success of the treatment regimen in this case was not solely due to the surgical procedure. A critical factor was the close cooperation among various medical experts who collectively navigated the challenging bits of diagnosis and treatment. When questions arise about a patient’s condition, it is essential to:
- Consult specialists who have deep experience with rare vascular anomalies.
- Utilize a blend of imaging techniques to get a comprehensive view of the pathology.
- Apply a careful, staged surgical protocol to mitigate risks and allow gradual recovery.
This integrated approach ensures that each subtle detail is given proper consideration. It also underscores the importance of continually updating diagnostic criteria and treatment protocols in response to emerging evidence from rare cases like this one.
Evaluating Modern Medical Imaging: Benefits and Challenges
Modern imaging techniques represent one of the biggest leaps forward in healthcare in recent years. While MSCT and colonoscopy allowed the medical team to get into the hidden complexities of the condition, they also come with challenges that are worth noting.
Some of the challenges and benefits include:
-
Benefits:
- High-resolution images that capture the fine details of vascular lesions.
- Ability to view both the superficial and deeper layers of affected tissues.
- Enhanced accuracy in planning surgical interventions.
-
Challenges:
- Interpreting the images correctly requires expertise—a slight difference in density readings may change the diagnosis.
- Integration of findings from different imaging modalities can be nerve-racking if the results do not align clearly.
- Accessibility to state-of-the-art imaging equipment is not universal, which can make it hard to manage such cases in less specialized settings.
Despite these challenges, modern techniques continue to build our collective ability to diagnose and treat complicated vascular malformations. They also serve as a reminder that ongoing professional training and investment in advanced medical technologies are key to improving patient outcomes.
Patient Experience and the Broader Implications for Healthcare Providers
The personal perspective of the patient involved in this case contributes greatly to the overall narrative. Facing recurrent symptoms for years without proper diagnosis can be both intimidating and disheartening. It highlights the necessity for healthcare providers to maintain open lines of communication, ensure thorough follow-ups, and deliver care that takes the patient’s experience into account.
Patients with complex conditions like this one often report that:
- They feel more reassured when their healthcare team takes the extra step of double-checking symptoms that might initially seem typical but then turn out to be part of a larger pattern.
- Receiving explanations that connect the dots between subtle physical signs and actual pathological findings makes the diagnostic journey less overwhelming.
- A clear, staged treatment plan alleviates concerns about unexpected complications during surgery and postoperative recovery.
For many patients, knowing that the surgical team had a thorough plan not only helped them trust the process but also provided peace of mind during their recovery. When patients are empowered with knowledge and are kept informed about every step, the overall treatment satisfaction is significantly improved—transforming what could be a nerve-racking experience into a more manageable one.
Combining Patient Insight with Modern Medical Practices
This case reinforces that the patient’s point of view is super important when designing treatment strategies. Beyond the technical aspects, the following elements were crucial for ensuring satisfaction:
- Informed Consent and Transparency: The patient was briefed thoroughly about the treatment plan, making it clear that each stage was necessary for successful management of the condition.
- Customized Care Plans: Recognizing that each case is unique, the medical team tailored the surgical approach to tackle the specific challenges posed by the lesion’s location and the vascular anatomy involved.
- Postoperative Support: Quick recovery protocols, early mobilization, and close monitoring of wound healing played key roles in ensuring a smooth recovery.
By integrating patient insights with clinical expertise and technological advancements, healthcare providers can better address even the most challenging cases. This holistic approach not only optimizes clinical outcomes but also ensures that patients leave the hospital feeling assured and valued.
The Future: Embracing a Collaborative and Evolving Treatment Landscape
This case study pushes us to consider the future of managing rare and complicated vascular malformations. There is an ongoing need for collaborative research and data-sharing amongst specialists in vascular anomalies. Continued advancements in medical technology—especially in imaging and minimally invasive surgery—will undoubtedly enhance our ability to diagnose and manage similar cases more accurately and with less discomfort for patients.
Future Directions in Diagnostics and Surgical Management
Looking ahead, several areas seem promising in refining how such conditions are approached:
-
Refined Imaging Techniques:
There is potential for even more detailed imaging modalities that could combine the benefits of MSCT and MRI, enabling physicians to get into the subtle details of tissue composition without invasive procedures.
-
Personalized Medicine:
Advances in genetic research and biomarker identification may eventually allow clinicians to predict who might be at risk for such rare forms of vascular malformations, prompting even earlier intervention.
-
Enhanced Surgical Tools:
With the evolution of robotic-assisted surgery and further improvements in laparoscopic instruments, future surgical interventions may become even more precise, lowering recovery times and reducing overall surgical risks.
-
Interdisciplinary Collaboration:
Encouraging stronger relationships between radiologists, pathologists, surgeons, and even experts in alternative medicine and nutrition could foster a truly holistic approach to patient care. This partnership can ensure that even the little twists and subtle details in a patient’s condition are not missed.
The promising future in healthcare is built on the foundations of modern surgical practices, a deep understanding of medical imaging, and the ongoing collaboration between specialties. As new research emerges, it will be critical for clinicians to remain open to integrating these latest findings into their diagnostic and therapeutic strategies.
Lessons Learned from This Unusual Case
There are several key lessons drawn from this case that can inform and guide future practice:
-
Stay Attentive to Uncommon Presentations:
Not all patients with recurrent rectal bleeding have common hemorrhoids. As this case illustrates, even a long-standing condition can hide larger issues that require more in-depth investigation.
-
Invest in Comprehensive Diagnostics:
Utilizing multiple imaging modalities and engaging in thorough diagnostic work-ups can help doctors find their way through the tangled issues inherent in rare conditions.
-
Embrace a Multidisciplinary Approach:
An integrated team approach is essential. When specialists across domains collaborate, the chances of overlooking a problematic detail are greatly reduced, leading to better overall patient outcomes.
-
Educate Patients and Encourage Regular Check-ups:
Patients should be encouraged to seek medical advice as soon as unusual symptoms appear. Regular follow-ups and awareness can prevent complications that arise from delayed diagnosis.
The integration of these strategies paves the way for improved patient care. For healthcare providers, the case offers not only a lesson in the importance of detailed imaging and staged surgical intervention but also a reminder that complex conditions can sometimes be managed successfully with modern minimally invasive techniques.
Conclusion: Bridging Clinical Insight with Patient-Centered Care
In closing, the case of the 45-year-old patient with Klippel-Trenaunay Syndrome and isolated rectal vascular malformation serves as a powerful reminder of the nuances inherent in diagnosing and treating rare vascular conditions. The journey from initial symptoms to definitive surgical treatment was filled with improbable twists and turns, requiring a balanced mix of advanced imaging, thorough pathology, and skilled surgical intervention.
What makes this case especially significant is how it challenges both patients and clinicians to re-examine what might seem like routine presentations. When conventional treatments fail or when recurring symptoms persist, it is crucial to dig into the fine points of the patient’s history and to employ comprehensive diagnostic methods that leave no stone unturned.
Moreover, the staged surgical approach illustrates that modern medicine is capable of adapting to even the most intimidating anomalies. By combining temporary measures—such as vena cava filters—with minimally invasive surgical techniques, healthcare providers can manage even complicated vascular malformations effectively. Such approaches demonstrate that when you work through the challenging bits with careful planning and a multidisciplinary strategy, both diagnostic and therapeutic success are well within reach.
This case also highlights the broader implications for a system-wide commitment to patient-centered care. Educating patients about the importance of follow-up care, ensuring that medical personnel remain up-to-date with the latest diagnostic protocols, and fostering a team-based approach to treatment are all essential components in transforming a nerve-racking situation into a manageable journey toward recovery.
Looking to the future, continued research and technological advancements are expected to further improve outcomes in similar cases. As imaging techniques become even more refined and surgical tools become more precise, the ability to detect and treat such rare vascular malformations will only improve. The lessons learned here can serve as a starting point for further innovation and collaboration, reinforcing the idea that medicine is as much about learning from the past as it is about embracing the future.
Ultimately, this case stands as an example of how intricate patient conditions can often be sorted out successfully when caution, collaboration, and modern techniques come together. It reminds us all that even in a field loaded with tricky parts and complicated pieces, the key to effective treatment lies in a thorough understanding of the condition, a willingness to adjust the treatment strategy as needed, and above all, a commitment to the well-being of the patient.
The success of this treatment, as well as the positive patient feedback regarding the method, encourages further dialogue among healthcare professionals. It is a call to action for continued investment in advanced diagnostic tools, enhanced training for clinicians, and improved interdisciplinary cooperation—all of which will pave the way for better care in the future.
In summary, the isolated rectal vascular malformation in a patient with Klippel-Trenaunay Syndrome may be rare, but its management is a testament to modern medicine’s ability to figure a path even when faced with unexpected or overwhelming challenges. As we reflect on this case, let it be a reminder that paying attention to small distinctions and subtle parts can often be the difference between a correct diagnosis and a missed opportunity for intervention.
Healthcare providers must remain vigilant. In an era where medical information and technology are continually advancing, it is essential to step back, review the evidence carefully, and adopt a holistic approach to treatment. This case, with all its tangled issues and innovative solutions, underscores that a patient-centered approach—along with the judicious use of modern technology—remains the most effective way to reach successful outcomes even in the most challenging scenarios.
Ultimately, the dialogue sparked by this unusual case should lead to more robust research, increased professional education, and ultimately, improved patient care on a broad scale. As we move forward, integrating lessons from rare cases with everyday clinical practice will help all of us—practitioners and patients alike—navigate the unpredictable but fascinating landscape of medical science.
Originally Post From https://www.dovepress.com/isolated-colorectal-involvement-in-klippel-trenaunay-syndrome-a-case-o-peer-reviewed-fulltext-article-IMCRJ
Read more about this topic at
Rectal arteriovenous malformations with acute …
Rectal Vascular Malformation