Reassessing Coronary Artery Calcium Scoring in Preventive Cardiology
Coronary artery calcium (CAC) scoring has increasingly positioned itself as a key instrument for individual cardiovascular risk assessment. In recent years, many have begun to appreciate its role beyond traditional risk calculators. This opinion editorial examines how CAC scoring might reshape primary prevention, weighing its potential benefits against its challenges and considering the evolving influence of emerging artificial intelligence (AI) methods, cost implications, and evolving guidelines.
While traditional risk models have long been employed to estimate the likelihood of a cardiovascular event, the direct visualization of calcified plaques in the coronary arteries offers a tangible and measurable insight into an individual’s atherosclerotic burden. In this piece, we get into the discussion about whether CAC scoring is ready to change the way clinicians decide on statin and aspirin therapies, an issue that is increasingly relevant given the current debates over how to best assess risk among diverse patient populations.
The Rise of Coronary Artery Calcium Scoring: A Game-Changer in Primary Prevention
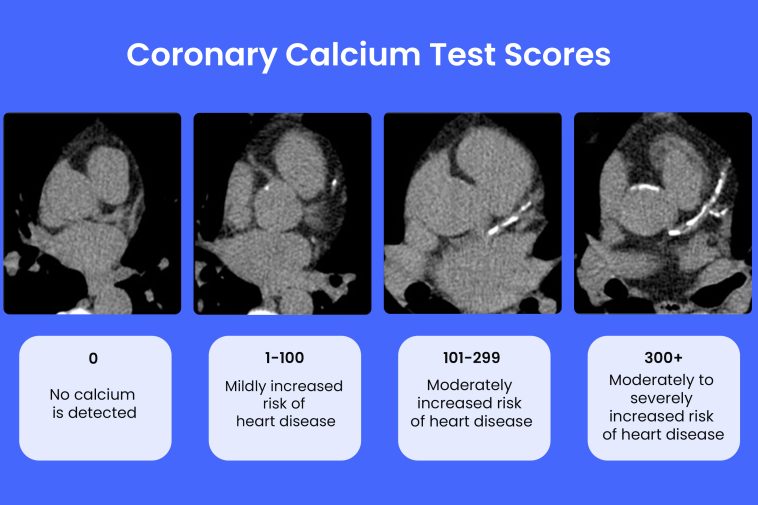
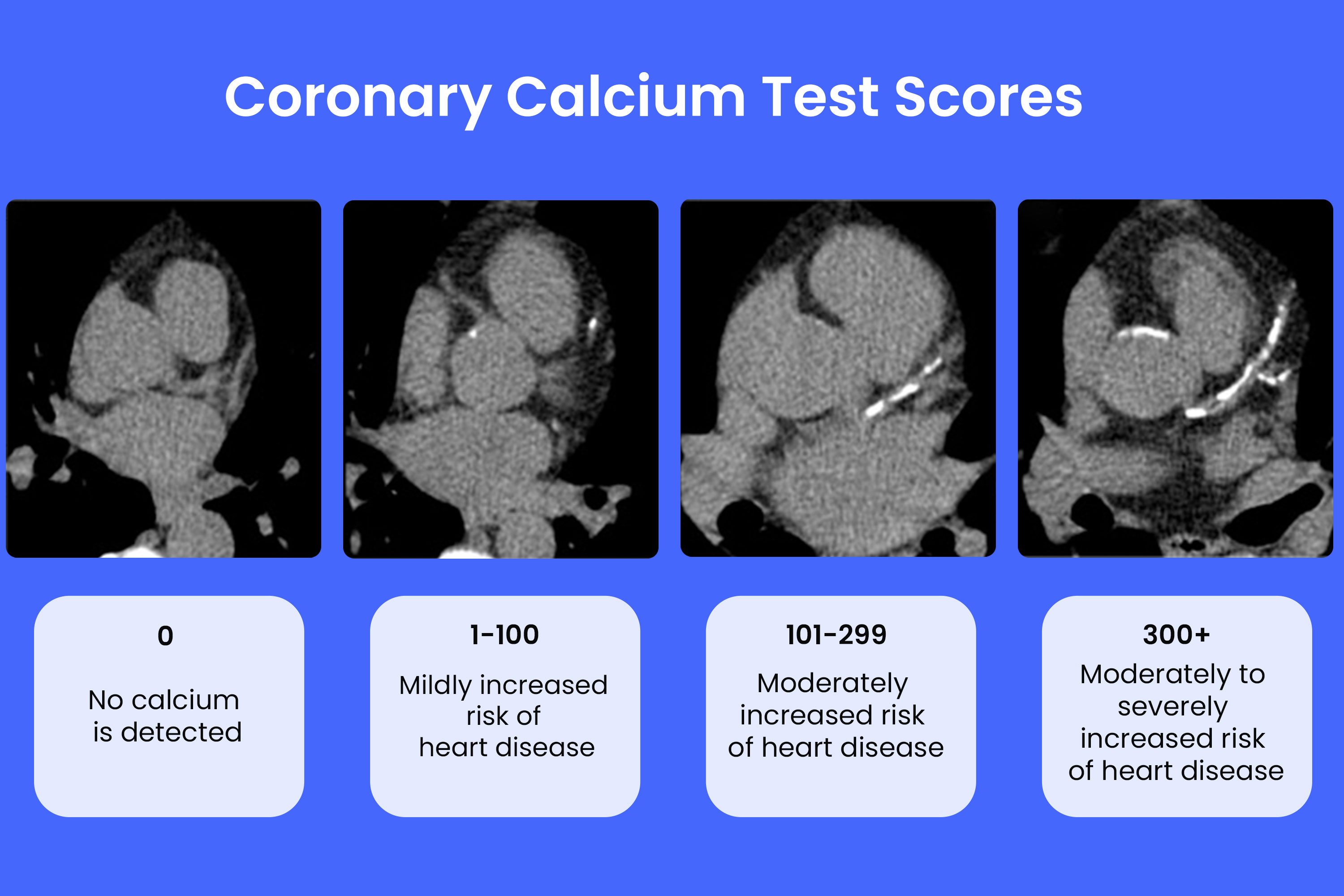
Over the last couple of decades, CAC scoring has emerged as an essential tool in preventive cardiology. As a non-invasive computed tomography (CT) technique, CAC scoring directly measures the calcified plaque present in coronary arteries. This direct measurement addresses many of the tricky parts associated with older risk prediction methods that only rely on clinical parameters such as blood pressure, cholesterol levels, and smoking history.
One of the key advantages with CAC scoring is its ability to provide a more personalized risk profile. Patients who might score in the intermediate risk range on traditional models may, in fact, be at significantly lower risk if their CAC score is zero. Conversely, individuals with several traditional risk factors but who show a CAC score higher than 100 often have a much greater risk, justifying a more aggressive preventive approach. In this sense, CAC scoring offers a tangible picture of the coronary state, which can help clinicians steer through treatment decisions with greater confidence.
With the inclusion of CAC in several recent guidelines—from the American College of Cardiology (ACC)/American Heart Association (AHA) to emerging recommendations in other regions—the test’s acceptance is growing. Still, many questions remain about its universal applicability, optimal implementation, and frequency of use, particularly when it comes to balancing its radiation exposure and cost with its prognostic power.
CAC Versus Traditional Risk Calculators: Fine Points and Small Distinctions
Traditional risk calculators such as the Framingham Risk Score, the HeartScore in Europe, and the pooled cohort equations (PCEs) have been indispensable in assessing the overall cardiovascular risk. However, these models are based mostly on demographic and clinical criteria, which sometimes obscure the hidden complexities of subclinical atherosclerosis.
Here are some key points that differentiate CAC scoring from its traditional counterparts:
- Direct Visualization: Traditional calculators infer risk based on indirect markers, while CAC scoring directly measures calcified plaque accumulation.
- Personalized Risk: A zero CAC score indicates extremely low event rates, which can help avoid unnecessary prescriptions and interventions, especially in patients with borderline risk.
- Incremental Prognostic Value: Studies have demonstrated that integrating CAC scoring with conventional risk factors improves overall prognostic accuracy and risk reclassification.
These small distinctions highlight how CAC scoring captures traits that traditional methods might miss. As a result, clinicians have a better chance of tailoring preventive therapies to each patient’s specific needs, thereby reducing the chances of overtreatment or undertreatment.
Tackling the Tricky Parts: Barriers and Confusing Bits in CAC Implementation
Despite its promising potential, deploying CAC scoring broadly in clinical practice is not without its tangled issues. The following points illustrate some of the challenging aspects encountered when integrating CAC into routine preventive cardiology:
- Guideline Discrepancies: Differences between major guidelines (e.g., ACC/AHA versus European Society of Cardiology) can make it nerve-racking for physicians to confidently adopt CAC-based strategies.
- Radiation Concerns: Even though the radiation dose from a CAC scan is relatively low (approximately 1 mSv), the cumulative effects in serial testing may be off-putting for some patients.
- Cost and Access: CAC scans are not universally accessible and their cost-effectiveness varies by region and patient subgroup, making the decision to use them a sometimes overwhelming proposition.
- Operational Hurdles: Variability in scan protocols, differences in equipment, and the need for specialized training further complicate its routine use.
It is crucial for healthcare providers to get into these topics and address them head-on by developing standardized protocols. Uniform training, clearer reimbursement criteria, and better integration into clinical workflows could help figure a path that reduces these confusing bits and boosts overall adoption.
Balancing Benefits and Risks: Guiding Statin and Aspirin Therapy Decisions
One of the most attractive applications of CAC scoring lies in its potential to better direct the use of both statins and aspirin. Rather than relying solely on estimated risk from background factors, CAC provides real-time insights into the subclinical plaque burden that can inform these decisions.
For instance, patients with a CAC score of zero generally have very low event rates. In such cases, initiating statin therapy might do more harm than good, particularly if patients are exposed to unnecessary medication side effects. Conversely, patients with scores exceeding 100 have a higher likelihood of adverse events, making them prime candidates for early statin initiation and—as long as bleeding risks are low—for aspirin therapy too.
A summary table of treatment recommendations based on CAC scores can help simplify these tricky parts:
| CAC Score Range | Statin Recommendation | Aspirin Recommendation | Notes |
|---|---|---|---|
| 0 | May defer statin therapy | Generally not recommended | No detectable plaque; focus on lifestyle modifications |
| 1–99 | Consider statins particularly if other risk factors are present | Not routinely recommended | Low to moderate plaque burden; decisions should factor in patient age and risk enhancers |
| >100 | Recommend statin therapy | May consider low-dose aspirin if bleeding risk is low | High risk; fast-track to preventive treatment |
By incorporating such a framework into clinical practice, physicians can better manage the small distinctions between different risk categories and make informed choices that align closely with individual needs.
The Economics of CAC Scanning: Weighing Cost-Effectiveness and Healthcare Impact
Any discussion about expanding the use of advanced diagnostic tools must also consider the economic side of things. While CAC scans can be slightly more expensive than relying solely on conventional risk evaluations, their cost-effectiveness becomes clearer when the long-term benefits are considered.
In several countries, studies have shown that CAC-guided treatment strategies offer acceptable incremental cost-effectiveness ratios (ICERs), especially among intermediate-risk populations. For example, in Australia and parts of the United States, the expense of a CAC scan may be offset by reductions in unnecessary medication, fewer side effects, and a decrease in emergency cardiovascular events.
Consider the following bullet list summarizing some key economic benefits:
- Enhanced Risk Reclassification: Redefining a patient’s risk category can prevent overtreatment and save on long-term medication costs.
- Improved Therapy Adherence: Seeing tangible calcification data may motivate patients to stick to prescribed therapies and lifestyle changes, reducing future complications.
- Reduced Adverse Events: By avoiding statin or aspirin therapy in individuals unlikely to benefit, the overall healthcare expenditure on managing side effects is minimized.
These economic angles help underline how CAC scanning is not merely a clinical tool but could also be a cost-saving measure in the broader context of population health management.
The Future of AI in CAC Scoring: Automating the Process and Uncovering Hidden Complexities
Artificial intelligence is transforming how we approach many areas of medicine, and CAC scoring is no exception. With AI-driven technologies, radiologists and clinicians can now process scans more rapidly and with increased accuracy. Deep learning models are already proving their worth by reducing interpretation errors and standardizing measurements across varying systems.
Some of the benefits of automated CAC scoring include:
- Faster Turnaround: AI-based tools can complete CAC quantification in seconds, speeding up decision-making in busy clinical settings.
- Consistency Across Centers: By reducing human variability, these systems alleviate the confusing bits that emerge because of inter-observer differences.
- Broader Accessibility: Opportunistic screening—where AI detects CAC on routine CT scans performed for other reasons—can extend the test’s benefits to more patients without additional radiation exposure or expense.
Nonetheless, significant challenges persist. Many AI models are developed on homogeneous datasets and may require further validation across diverse populations. The long-term impact of relying on automated systems and their integration into hospital workflows remains an area of active investigation. Future improvements in these technologies could help smooth out the small twists and turns that currently limit broader adoption.
Addressing Research Gaps: Overcoming the Tangled Issues in CAC Utilization
While current studies provide robust evidence that CAC scoring adds predictive value, several research gaps demand further exploration. One area of continued debate is whether universal CAC screening should be adopted, or if a selective approach—in which only high-risk patients are screened—offers the best balance of benefit to cost. Despite the promising data, the literature is still full of problems when it comes to standardizing CAC thresholds across varied patient subgroups.
Some of the areas where more work is needed include:
- Younger Adults: With the low prevalence of calcification in individuals under 45, determining how best to incorporate CAC encourages digging into high-risk subgroups, such as those with a strong family history of early-onset coronary artery disease.
- Elderly Populations: In older adults, nearly everyone has some degree of calcification. Here, the challenge is to figure a path through the small distinctions in plaque burden that meaningfully affect outcomes.
- Gender and Ethnic Differences: Many existing studies have predominantly white male participants. More inclusive research that captures the subtle parts of risk among women and ethnic minorities is crucial.
- Longitudinal Impacts: Beyond short-term observational studies, randomized controlled trials are needed to clarify whether CAC-guided treatment can indeed lower major adverse cardiovascular events (MACE) over the long term.
Addressing these gaps will require not only further studies but also an openness to recalibrating guidelines based on new data. By acknowledging the tangled issues and striving for standardization, the medical community can move toward a more equitable and effective use of CAC scoring.
Practical Recommendations: Finding Your Way Through the CAC Debate
This discussion is more than academic—it has real implications for everyday clinical practice. Here are several practical recommendations for clinicians and policymakers when it comes to integrating CAC scoring into routine care:
- Educate and Train Clinicians: Develop accessible training modules that cover the fine points of CAC interpretation and the small distinctions in treatment thresholds.
- Standardize Protocols: Collaborate among professional societies to reduce guideline discrepancies. Establish universal thresholds that can be used across institutions.
- Integrate AI Thoughtfully: Merge AI tools with existing clinical workflows to ensure consistency and reliability, all while keeping an eye on ethical standards and regulatory approvals.
- Encourage Inclusive Research: Sponsor studies that include underrepresented groups, such as young adults, women, and diverse ethnic backgrounds, to ensure that findings are broadly applicable.
- Consider Cost-Effectiveness: Evaluate the local economic context to determine which patient populations would benefit most from CAC-guided therapy, taking into account both direct scan costs and potential long-term savings.
When clinicians and health systems work together on these fronts, the intertwined benefits of personalized care and cost-effective prevention will likely outweigh the initial challenges.
Patient Perspectives: Communicating Risk and Ensuring Informed Decisions
The successful implementation of CAC scoring in preventive cardiology not only depends on clinical guidelines and economic factors but also on effective communication with patients. Often, discussions around preventing heart disease can become overwhelming or even scary due to the number of tests and potential side effects of treatments like statins and aspirin.
When talking with patients, healthcare providers can consider the following approaches:
- Keep It Simple: Use clear language and relatable analogies to explain what a CAC score means. For example, compare it to a snapshot of the “clogging” in the arteries.
- Discuss Personalization: Emphasize that a zero CAC score might allow for a more relaxed approach, while a higher score would call for proactive therapy – all based on that patient’s own data.
- Focus on Lifestyle: Highlight that along with medications, lifestyle modifications remain a critical component of heart disease prevention. Diet, exercise, and smoking cessation are all essential strategies.
- Explore the Options: Ensure patients understand both the benefits and the potential challenges (e.g., incidental findings or radiation exposure) so they feel informed and involved in the decision-making process.
Patient-centered communication not only builds trust but also minimizes the nerve-racking bits of the evaluation process. By focusing on clear, compassionate dialogue, clinicians can help patients feel empowered to take charge of their cardiovascular health.
Integrating CAC Into Broader Healthcare Strategies
CAC scoring’s true power may only be fully realized when it is integrated into a larger preventive framework. This means not treating CAC as a standalone metric but rather as one part of a multi-faceted approach that includes:
- Enhanced Electronic Health Records (EHR): Embedding CAC scores into patient records, ideally integrated with decision support systems, ensures that all team members are on the same page.
- Multidisciplinary Collaboration: Cardiologists, primary care providers, radiologists, and even AI specialists can work together to create a cohesive care pathway that optimizes both screening and subsequent interventions.
- Community Health Initiatives: In settings with limited resources, selectively applying CAC scanning in high-risk populations could become part of broader public health campaigns aimed at reducing heart disease.
By aligning CAC scoring with other risk reduction measures, healthcare systems can offer more comprehensive and personalized care. This more integrated approach not only addresses the specific coronary concerns but also contributes to overall improvements in population health.
Looking Ahead: The Future of Preventive Cardiology in a Changing Landscape
The landscape of preventive cardiology is full of twists and turns. As medical knowledge continues to expand and technologies such as AI reshape how we interpret data, the potential for more refined and personalized preventive strategies becomes ever more tangible. The future of CAC scoring appears promising if its implementation is coupled with focused research, enhanced clinician training, and standardized guidelines.
Several ongoing trials—like ROBINSCA, DANCAVAS, and CAC-PREVENTABLE—promise to provide further insights into the long-term clinical outcomes of CAC-guided strategies. In addition, as AI technology develops, we may soon see fully automated CAC scoring systems that are seamlessly integrated into daily radiological workflows. Such innovations would not only minimize the tangled issues of manual interpretation but also reduce the time required for image analysis, improving overall efficiency in busy clinical settings.
Looking forward, the integration of imaging biomarkers like CAC with other emerging indicators—such as polygenic risk scores and serum biomarkers—could mark the beginning of a new era in cardiovascular risk stratification. In this future, a more complete picture of heart disease risk will enable clinicians to tailor preventive interventions with unprecedented precision, ushering in an era of truly personalized medicine.
Conclusion
In summary, coronary artery calcium scoring is no longer a niche tool reserved for academic studies. Its rise as an integral component of primary prevention in cardiology demonstrates its potential to improve the accuracy of risk stratification and guide tailored therapies—especially regarding statin and aspirin use.
Though the path to full integration is loaded with challenges, from guideline discrepancies and radiation concerns to cost issues and the need for broader validation in diverse populations, the potential benefits are undeniable. CAC scoring offers a way to directly assess the extent of coronary atherosclerosis, thereby revealing hidden risk that may be missed by traditional risk calculators. This direct approach not only enhances preventive strategies but also contributes to more cost-effective care by potentially reducing overtreatment.
The future of this technology is closely intertwined with advances in artificial intelligence, which promises to streamline the entire process – reducing the nerve-racking bits of manual interpretation and helping bridge current gaps in consistency and standardization. As hospitals and practices adopt more integrated electronic health systems and better decision support tools, the opportunities for opportunistic screening and real-time risk classification will only expand.
Moving forward, key recommendations include increased clinician education, the development of unified testing protocols, and greater efforts to include underrepresented groups in research. These efforts are toward ensuring that every patient, regardless of age, gender, or ethnic background, benefits from a personalized and equitable approach to cardiovascular risk assessment.
Ultimately, by taking a closer look at the evidence and striving to figure a path through the challenging bits, the medical community can harness the full potential of coronary artery calcium scoring. The integration of this tool, when combined with other preventive measures, holds the promise of redefining cardiovascular risk management and paving the way for improved long-term outcomes in heart health.
As with all evolving technologies and strategies, the journey is ongoing. However, if we continue to address the tangled issues, streamline operational hurdles, and integrate emerging AI innovations, CAC scoring could firmly secure its place as a cornerstone of personalized preventive cardiology. The time is ripe for embracing this powerful tool, and the future looks both exciting and promising for those willing to navigate its twists and turns with a balanced perspective.
Originally Post From https://www.cureus.com/articles/410752-beyond-traditional-risk-calculators-the-expanding-role-of-coronary-artery-calcium-scoring-in-preventive-cardiology
Read more about this topic at
MESA Risk Score and Coronary Age Calculator
Coronary calcium scan