The Promise and Pitfalls of Stroke Prevention After Atrial Fibrillation Ablation
The OPTION trial has sparked intriguing discussions in the medical community about the best stroke prevention approaches following atrial fibrillation (AF) ablation. Recent subanalyses from this pivotal study provide valuable insights into how left atrial appendage closure (LAAC) measures up against oral anticoagulation (OAC) in patients with varying degrees of stroke risk. As many healthcare professionals seek treatment options that minimize bleeding while preserving the benefits of stroke prevention, these findings challenge us to rethink current protocols. In this opinion editorial, we’ll get into the study’s outcomes, reflect on the practical implications, and discuss what these results could mean for the future of AF management.
Notably, the trial analyzed a group of nearly 1,600 patients with a moderate to high risk of stroke based on the CHA₂DS₂-VASc score. The participants were split into two groups—those receiving LAAC using the Watchman FLX device, and those continuing OAC therapy. With a follow-up period of 36 months, the study observed that LAAC was as effective as OAC in preventing stroke and systemic embolism, while also delivering the added bonus of significantly lower bleeding events. This has important real-world implications, particularly for patients who face challenges in maintaining long-term blood thinner regimens because of bleeding complications.
Taking a Closer Look at the OPTION Trial Outcomes
The OPTION trial’s design and execution were relatively straightforward, yet the trial’s outcomes contain plenty of tricky parts and subtle details that require a deeper understanding. Conducted at multiple centers across notable regions including Abu Dhabi, Canada, Florida, London, Nevada, and Ohio, the trial managed to capture diverse patient backgrounds while keeping its focus on the comparative safety and effectiveness of LAAC versus OAC.
In the trial, investigators particularly emphasized two primary endpoints: safety and efficacy. The safety endpoint was focused on nonprocedural major or clinically relevant nonmajor bleeding, whereas the efficacy endpoint relied on a composite measure that consolidated all-cause death, stroke, or systemic embolism. LAAC demonstrated superiority in reducing bleeding by demonstrating an 8.5% occurrence rate compared to 18.1% in the OAC group—a key statistic that reflects its potential to reduce complications in certain high-risk patients.
Key Findings at a Glance
| Parameter | LAAC Group | OAC Group |
|---|---|---|
| Nonprocedural Bleeding | 8.5% | 18.1% |
| Composite Efficacy Endpoint (Death, Stroke, Systemic Embolism) | 5.3% | 5.8% |
This table provides an at-a-glance understanding of the primary outcomes, highlighting that LAAC is not only comparable in efficacy but offers a secondary benefit of reduced bleeding. These outcomes are particularly compelling for patients who are on the receiving end of either therapy, especially when the bleeding risk is a critical consideration in their treatment plans.
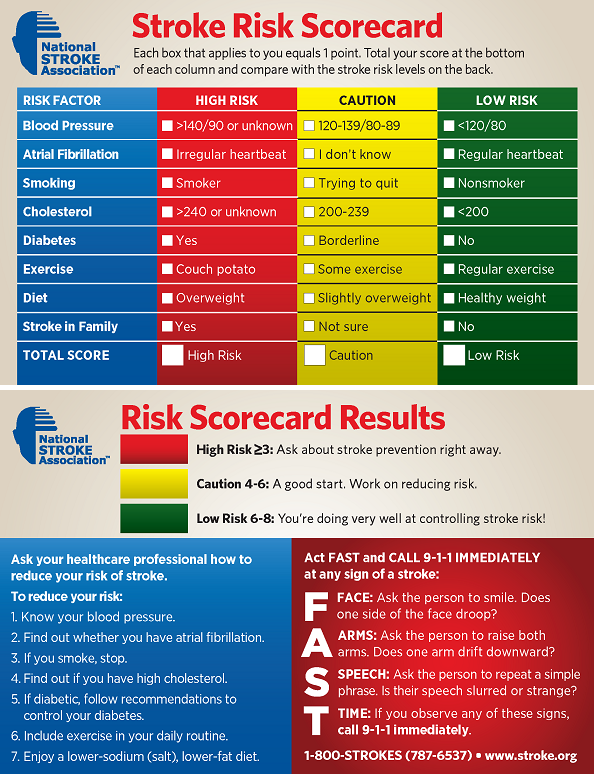
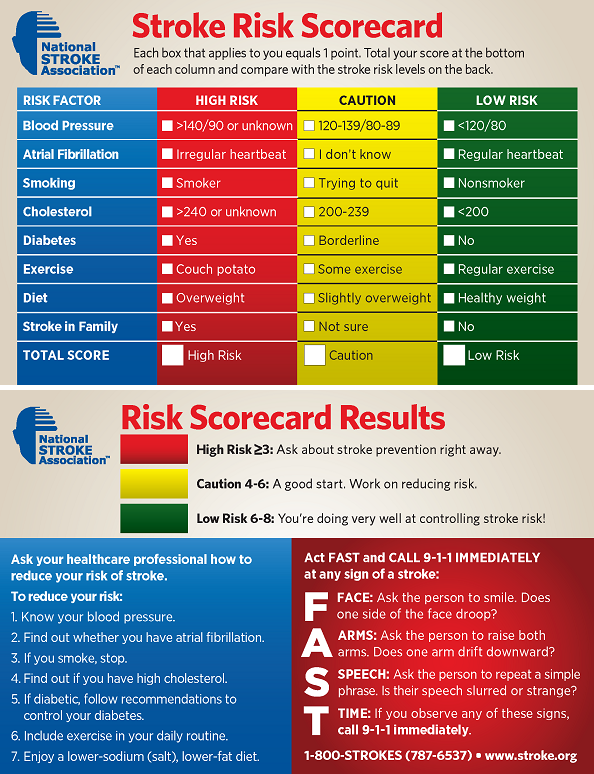
Understanding Stroke Risk: Breaking Down the CHA₂DS₂-VASc Scale
The CHA₂DS₂-VASc scale is a cornerstone in stroke risk assessment for patients with atrial fibrillation. It ranges from 0, indicating a lower risk, to 9, reflecting an elevated stroke risk. What’s interesting to note is that in the OPTION trial, all patients had scores that indicated at least a moderate risk of stroke. As a result, the trial included patients who had scores of 2 for men and 3 for women as a baseline for entry.
For the purposes of the subanalysis, stroke risk was sorted into two groups based on a threshold score of 4. Patients scoring 4 or more were classified as high risk, while those scoring 3 or below were considered to be at lower stroke risk. Although more than 90% of the trial population scored between 2 and 5, subtle distinctions between the outcomes for high and low stroke risk groups were examined. This breakdown plays a key role in understanding how best to figure a path forward when recommending treatment strategies.
Patient Demographics and Their Impact
The subanalysis also revealed interesting demographic trends. Patients with higher scores tended to be predominantly female and older (≥75 years), with a greater number of accompanying comorbidities. The fact that patient characteristics such as age and the presence of other health conditions might influence outcomes is an important consideration for clinicians who are trying to steer through the many factors involved in stroke prevention.
Here is a summary of the demographic data by treatment group for clarity:
- High Stroke Risk (CHA₂DS₂-VASc score ≥4): Approximately 370 patients in the LAAC group and 368 in the OAC group.
- Lower Stroke Risk (CHA₂DS₂-VASc score ≤3): Around 433 patients in the LAAC group and 429 in the OAC group.
This balanced distribution ensures that the trial results can be considered robust across a wide range of patients, even though few participants fell at the extreme ends of the stroke risk spectrum. For those patients considered particularly vulnerable, even the slight differences in patient characteristics can lead to big decisions about choosing one therapy over another.
Digging Into the Tricky Parts of Treatment Selection
At the heart of the ongoing debate is the trade-off between maintaining effective stroke prevention and managing the risk for potentially overwhelming bleeding events. Oral anticoagulation has long been the standard of care, but it carries with it the nagging concern of bleeding complications—a matter that can be both intimidating and nerve-racking for patients and physicians alike. On the other hand, LAAC offers a compelling alternative that sidesteps the need for continuous anticoagulation, thereby reducing bleeding risks significantly.
However, the decision is far from simple. Clinicians must consider the numerous small distinctions in both efficacy and safety, including the potential for procedural bleeding during LAAC implantation, which, although occurring at low rates (approximately 1% across the board), still remains a parameter requiring cautious evaluation.
To put it simply, while LAAC shows promise as a substitute for OAC for many patients, especially those who have had complications on blood thinners, it is not without its nuanced challenges. The choice between continued pharmacological therapy and a device-implanted approach needs to be individualized, weighing the minor twists and turns inherent in each treatment option.
Comparing Efficacy: LAAC Versus OAC Across Stroke Risk Levels
The OPTION trial offers clear evidence that, regardless of whether patients had a higher or lower calculated stroke risk, the composite effectiveness endpoint—combining outcomes like stroke, systemic embolism, and death—showed no significant difference between LAAC and OAC. This finding reinforces the idea that both treatments are comparably effective over a three-year period.
For many patients, this means that the choice of treatment could lean towards the option that minimizes other risks. In this case, LAAC has the added advantage of reducing the chance of nonprocedural bleeding events. The results clearly indicate that in patients at both high and lower stroke risk, the benefit of fewer bleeding events with LAAC makes it a super important alternative for those who struggle with the tricky parts of long-term blood thinner use.
Bullet Points of Key Comparative Outcomes
- Efficacy Equivalence: Both LAAC and OAC resulted in comparable rates of death, stroke, and systemic embolism.
- Bleeding Complications: LAAC group experienced significantly lower rates of nonprocedural (primarily clinically relevant nonmajor) bleeding compared to the OAC group.
- Consistent Benefits: The reduction in bleeding risk was maintained across both high and lower stroke risk populations.
- Risk Factor Balance: The trial’s randomization process ensured a balanced representation of patient demographics, helping clinicians better figure a path in tailoring treatment strategies.
These bullet points summarize the findings in a digestible format and underscore the potential for LAAC to be a game changer for patients who are particularly sensitive to bleeding complications from oral anticoagulants. Still, it is crucial that both the subtle parts of these alternatives are discussed extensively with patients during treatment planning.
Charting a Course Through Post-AF Ablation Treatment Options
For many cardiologists, the decision to continue anticoagulation after a successful catheter ablation is not always straightforward. Understanding the fine points involved in these treatment pathways is essential, especially when hopes are pinned on preventing thromboembolic events. The OPTION trial, with its extensive follow-up and focus on both efficacy and safety, provides a comprehensive look at these issues.
The subanalysis specifically aimed to compare outcomes based on the CHA₂DS₂-VASc score. The design of the trial allowed a closer look into these subtle differences by stratifying patients into distinct risk categories. For many physicians, this means they can now offer LAAC with a higher degree of confidence—knowing that even in patients deemed at high risk for stroke, the reduction in bleeding incidents remains significant. This nuanced approach is particularly valuable for patients who may be unable to continue long-term blood thinning medications due to past bleeding episodes or other complications.
Considerations for Clinicians and Patients Alike
When making therapeutic decisions, both clinicians and patients must keep several factors in mind:
- Individual Patient Risk: A patient’s age, sex, and concomitant conditions can significantly influence the benefits or drawbacks of either treatment.
- Tolerance to Medication: For patients who experience uncomfortable or even dangerous bleeding events on OAC, LAAC offers a practical alternative.
- Long-Term Implications: The long-term safety profile of the chosen therapy is critical. LAAC has shown a stable performance over 36 months, which can ease some concerns about the durability of the results.
- Personal Preferences: In today’s patient-centered care model, the treatment decision should respect the individual’s quality of life, concerns about bleeding, and willingness to undergo a device implantation procedure.
These considerations highlight that choosing between LAAC and OAC often involves managing your way through several intertwined factors. Each patient’s unique situation—their comorbidities, their comfort with procedural risks, and their capacity to adhere to a medication regimen—must be weighed carefully. In practice, this means that clear communication and shared decision-making are indispensable tools for both managing expectations and optimizing outcomes.
Together, We Must Address the Hidden Complexities in Stroke Prevention
The OPTION trial’s results inevitably prompt us to pay attention to the subtle parts of stroke prevention in the context of atrial fibrillation ablation. For years, the reliance on oral anticoagulation has been a given; however, not every patient can safely make that leap without facing the nerve-racking possibility of bleeding complications. Now, with LAAC emerging as a viable and effective alternative—even for those at the highest risk—it becomes essential to reassess and potentially broaden our treatment paradigms.
Still, while the promise of LAAC is evident, there are several tricky parts that continue to require further research. One should note that the trial was not fully powered to draw absolute conclusions on every primary endpoint—especially in very high or very low risk cohorts. This means that while the data is compelling, it is also layered with some of the confusing bits that inherently accompany long-term clinical research.
Strengths and Limitations: A Balanced Perspective
While the trial’s strengths include a robust sample size, a balanced randomization process, and clear benefits in reduced bleeding, it is equally important to acknowledge the trial’s limitations:
- Sample Size in Extreme Cases: Few patients fell at the extreme ends of the CHA₂DS₂-VASc spectrum, which means that outcomes for these very high or very low risk groups remain somewhat uncertain.
- Procedural Considerations: Though the device implantation yielded low procedural bleeding (around 1%), there is still an undeniable narrative around procedural risks that could be concerning to some patients.
- Long-Term Data Beyond 36 Months: While 36 months is a meaningful follow-up period, the long-term durability and safety of the LAAC device compared to chronic OAC usage warrants further study.
These points encourage clinicians and researchers alike to remain cautious and to continue our quest to figure a path through the many dimensions of stroke prevention. New research, extended follow-up studies, and innovative trial designs will all be key to better understanding the full range of benefits and potential pitfalls associated with LAAC.
Patient Perspectives: Quality of Life and the Road Ahead
While clinical data is indispensable, the qualitative impact on a patient’s life is equally critical. Many patients who have battled with the nerve-racking side effects of long-term oral anticoagulation ultimately suffer from the cumulative stress of managing their condition. In this context, LAAC may be perceived as a beacon of hope—a way to potentially sidestep the constant worry about bleeding risk while still maintaining robust stroke prevention.
For patients who have had to repeatedly deal with the fine points of managing medication adjustments, periodic monitoring, and the off-putting news of bleeding episodes, the simplicity of a one-time device placement is appealing. That said, the decision remains highly personal and should be individualized through thoughtful conversation and shared decision-making between patients and their healthcare providers.
What Patients Often Consider When Choosing Stroke Prevention Options
- Simplicity: Removing the need for daily or frequent medication may ease the confusing bits of managing a complex treatment regimen.
- Long-Term Safety: The promise of reduced bleeding is particularly attractive to patients who have a history of, or anxiety about, bleeding episodes.
- Practicality: A one-time or short-duration intervention can be preferable for patients who worry about the twist and turns of long-term pharmaceutical management.
- Immediate Versus Future Benefits: Some patients value immediate reductions in risk, while others concentrate on how a treatment can impact their quality of life over many years.
These subtle details highlight that the road to recovery and stroke prevention is as much about personal comfort as it is about clinical outcomes. By offering a viable alternative like LAAC, healthcare providers empower patients to choose a treatment that aligns with both their medical needs and their lifestyle preferences.
Looking Beyond the Numbers: The Broader Implications for Modern Medicine
Modern medicine is continuously evolving, and the OPTION trial represents a modern milestone. It challenges the conventional wisdom that long-term oral anticoagulation is the only path to optimal stroke prevention in patients post-AF ablation. For many years, clinicians have wrestled with the tangled issues that come from relying solely on medication. There is now an opportunity to broaden our perspectives and embrace technologies that serve to reduce the complications associated with chronic therapy.
There is also a larger narrative here about alternative approaches in medicine. LAAC is one example of how modern devices and procedural innovations can offer a different path that sidesteps some of the intimidating risks of traditional pharmaceutical therapies. While every medical solution has its own set of complicated pieces, the ability to choose an approach that minimizes one risk while providing similar overall benefits is a development that cannot be ignored. For many, this means we might soon see a shift in how stroke prevention is approached in the context of AF ablation.
Insights Into Future Research Directions
As with every breakthrough, further research is essential. Future studies should focus on:
- Extended Follow-Up: Monitoring outcomes beyond 36 months to ensure that the benefits of LAAC continue over the long haul.
- Wider Patient Populations: Including more patients with the extreme ends of the stroke risk spectrum to better grasp the overall safety profile.
- Comparative Studies with Other Devices: As more LAAC technologies emerge, cross-comparisons will be crucial in identifying the most effective and safest options.
- Cost-Effectiveness Analyses: With healthcare budgets under constant pressure, understanding the economic impact of switching from OAC to LAAC can facilitate broader acceptance of this new strategy.
Each of these future research avenues will help in clarifying the fine shades of differences between various treatment modalities. With every study, we are getting a bit closer to a more personalized healthcare approach that considers both clinical effectiveness and patient preferences.
Managing Your Way Through Clinical Decision-Making: A Clinician’s Perspective
For physicians and healthcare providers, the OPTION trial doesn’t just provide hard numbers and statistics—it offers a framework for managing your path through post-ablation treatment choices. Many clinicians often face the overwhelming task of balancing efficacy with safety in patients who carry a high burden of comorbidities and risk factors. The low bleeding rates observed with LAAC serve as a key reassurance, particularly for patients who find long-term blood thinners both intimidating and burdensome.
In practical terms, the trial reaffirms that LAAC is a comparable alternative for stroke prevention with distinct advantages in bleeding outcomes. This should encourage physicians to consider device closure not only as a backup plan but as a primary candidate for patients likely to struggle with the fine points of anticoagulation therapy management. With shared decision-making at the center of patient care, clinicians now have another tool in their arsenal to tailor treatments that suit individual patient profiles.
Steps Clinicians Can Take to Personalize Patient Care
- Risk Assessment: Use risk tools like the CHA₂DS₂-VASc scale to gauge stroke risk accurately.
- Patient Education: Clearly explain the relative risks of bleeding with OAC versus the procedural risks and benefits of LAAC.
- Shared Decision-Making: Incorporate patient preferences by discussing what matters most—quality of life, ease of treatment, and risk of side effects.
- Ongoing Monitoring: Ensure that whichever treatment is chosen, patients are closely monitored to catch any subtle issues early.
This approach ensures that treatment plans aren’t one-size-fits-all, but rather are carefully adapted to suit the personal and clinical circumstances of each patient. It’s about working together, finding common ground between patient expectations and clinical realities, and ultimately reaching a decision that minimizes overwhelming risks while maximizing benefits.
Embracing a New Era in Stroke Prevention Strategy
The OPTION trial’s results leave us with a clear message: modern treatment options for stroke prevention in the context of AF ablation have evolved to the point where LAAC offers a strong alternative, particularly for patients who are troubled by the nerve-racking side effects of ongoing oral anticoagulation. As clinical practice continues to advance, we need to be open to incorporating new technologies and personalized treatment plans that elevate patient care and reduce the tangled issues associated with traditional therapies.
It is critical that we continue to dig into emerging data, compare our current practices with innovative alternatives, and steer through the many intersecting factors that determine treatment success. The trial’s demonstration that LAAC can provide comparable long-term stroke prevention, yet with the added benefit of reduced bleeding complications, is a call to action for the medical community to reexamine how we conceptualize and deliver stroke prevention therapy.
The Impact on Healthcare Policy and Practice
From a broader perspective, the trial’s outcomes have the potential to influence both clinical guidelines and healthcare policies. As evidence accumulates in support of LAAC for certain patient groups, we might see updates to national and international guidelines that reflect these newer, less burdensome approaches to stroke prevention. Policymakers, too, will need to weigh the economic implications alongside clinical benefits, striving to make advanced treatment options widely accessible and cost-effective.
Clinicians, administrators, and patients alike must adapt to these changing dynamics. With the increasing availability of devices like the Watchman FLX, and the steady stream of data supporting their use in high-risk populations, there is a real opportunity to improve outcomes in a segment of patients who have long been caught between effective stroke prevention and the intimidating risk of long-term anticoagulation therapy.
Final Thoughts: Balancing Efficacy, Safety, and Quality of Life
In summary, the OPTION trial has opened up an alternative path for stroke prevention that is both effective and associated with fewer bleeding events. For anyone involved in post-AF ablation care, whether as a clinician or a patient, these findings highlight the importance of looking beyond traditional treatment paradigms and embracing innovative strategies that align with modern medicine’s evolving landscape.
While every treatment option comes with its own set of tricky parts and hidden complexities, it is the willingness to compare these options, figure a path forward based on the best available data, and to engage in open, shared decision-making that will ultimately lead to improved patient outcomes. The results of the OPTION trial encourage us to think beyond a one-dimensional view of stroke prevention—reminding us that what works for one patient may not work as well for another, and that personalized care is super important.
Key Takeaways for a Modern Healthcare Approach
- Comparative Efficacy: LAAC provides stroke prevention that is on par with OAC in carefully selected patients.
- Reduced Bleeding Risk: The lower incidence of nonprocedural bleeding in LAAC is a notable advantage, particularly for those who have experienced bleeding issues on OAC.
- Patient-Centered Care: Treatment decisions should integrate patient preferences, risk profiles, and quality-of-life considerations.
- Future Research: Extended follow-up studies and broader patient population research are needed to solidify these findings further.
- Clinical Integration: Clinicians must balance the nerve-racking risks associated with long-term pharmacotherapy against innovative alternative strategies that promise fewer complications.
As we continue to adapt to the challenges posed by atrial fibrillation and stroke risk management, it’s essential to remain both flexible and proactive in our approach to patient care. Continuous research, combined with open discussions and shared decisions between healthcare providers and patients, will help us work through the fine points and subtle details of these complex treatment strategies. The OPTION trial has indeed paved the way for a new era in stroke prevention—one where efficacy, safety, and quality of life are all given their due importance.
Conclusion: A Brave New World of Stroke Prevention
The OPTION trial’s extensive subanalysis, when viewed through the lens of everyday clinical practice, offers a hopeful alternative for patients who find themselves torn between the promising protection of stroke prevention and the overwhelming risks of bleeding. While every treatment has its own tangled issues and twists and turns, the ability to choose LAAC as a primary option for post-AF ablation patients provides a refreshing change from the longstanding reliance on continuous administration of blood thinners.
What we take away from these findings is not just the efficacy and safety data, but the broader message that modern medicine must continue to innovate and personalize care. By taking a closer look at the comparative benefits and risks, and by carefully considering patient-specific factors using practical tools like the CHA₂DS₂-VASc scale, healthcare providers can create tailored treatment strategies that truly address the messy, real-world challenges of managing stroke risk.
Even as we acknowledge the limitations of the current data—particularly in the patient groups lying at the extreme ends of stroke risk—the overall trends are encouraging. With reduced bleeding complications, LAAC offers patients a treatment strategy that minimizes some of the intimidating aspects of long-term anticoagulation while still providing robust stroke prevention. As such, it represents a significant step forward in our ongoing effort to balance efficacy, safety, and quality of life in the battle against atrial fibrillation and stroke.
Ultimately, the discussion sparked by the OPTION trial is full of promise. It beckons us to continue refining our approaches, to compare different treatment methods actively, and to work together—patient and provider—to find the best path forward through the many subtle details and tricky parts of stroke prevention. In a medical landscape that is as dynamic as it is challenging, the light shed by these findings guides us toward a future where individualized, effective, and safe treatment is within reach for every patient.
Originally Post From https://consultqd.clevelandclinic.org/option-results-remain-consistent-regardless-of-stroke-risk-level
Read more about this topic at
Safety vs. efficacy assessment of pharmaceuticals
Evaluating Drug Efficacy and Safety – Clinical Pharmacology