Revisiting the Role of Tumor Pericytes in Metastasis: A Fresh Look at Vascular Dynamics
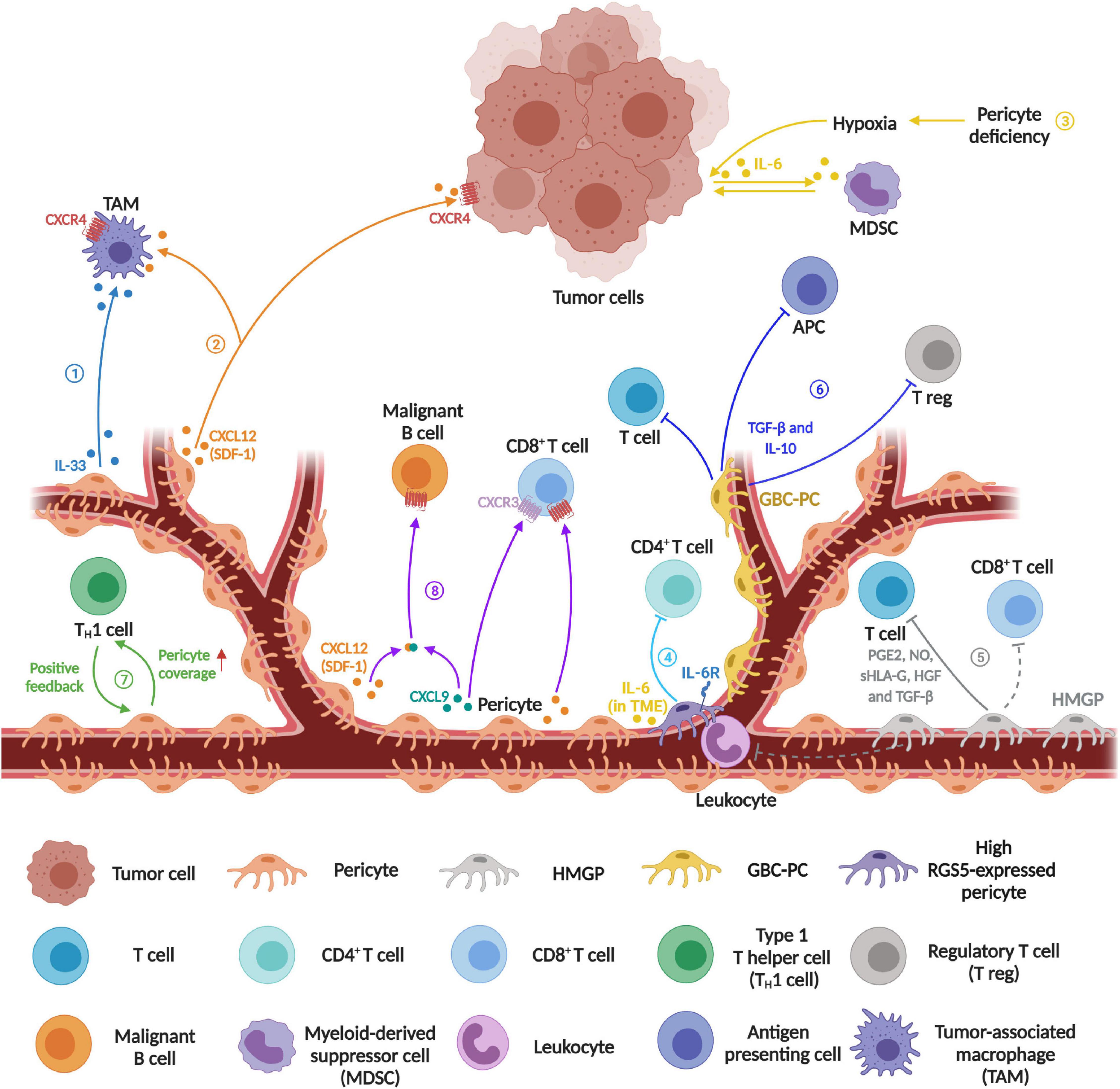
The latest research in oncology has begun to shine a light on the tricky parts of cancer spread. Recent findings reveal that tumor pericytes—cells that line blood vessels—are more than just bystanders. They play a crucial role in sculpting the local vascular tone and hemodynamics within tumors, ultimately facilitating the spread of cancer cells. In this editorial, we explore this study’s findings, the hidden complexities of pericyte regulation, and what it could mean for future cancer therapies. We also examine the role of noncoding RNA molecules and the potential of targeted therapeutic strategies aimed at these cells.
At first glance, the formation and structure of blood vessels in a tumor might seem straightforward. However, on closer inspection, there are numerous fine points and subtle twists and turns involved. The study we are discussing takes a closer look at how pericytes in tumors relax or contract, influencing blood flow and vessel permeability, thereby creating an environment that can assist cancer cells in leaving the primary tumor and invading other regions.
Understanding the Tumor Microenvironment: Vascular Tone and Hemodynamics in Metastasis
One of the key messages from this research is that the dynamics of blood flow (hemodynamics) in the tumor microenvironment are not random. Rather, these dynamics are regulated by the contraction and relaxation of pericytes. These cells, known for wrapping around the endothelial cells (which form the inner lining of vessels), are capable of changing the vessel diameter—a factor that directly influences blood flow speed and vessel leakiness.
The study revealed that tumors prone to liver metastasis exhibit a notable increase in local blood flow and an enlarged vessel diameter compared to non-metastatic tumors. Essentially, when the blood vessels relax and dilate, they not only allow a greater volume of blood to pass through but also create gaps between endothelial cells, making it easier for tumor cells to intravasate, or enter the bloodstream.
Key Elements of Tumor Vascular Tone Regulation
- Pericyte Contraction and Relaxation: Pericytes can contract or relax, which directly affects the vessel diameter and blood velocity. This process involves a cascade of intracellular signals where calcium ions play a pivotal role.
- Calcium Signaling: Calcium influx is one of the core determinants of pericyte contraction. When calcium channels are suppressed, pericytes relax, causing vasodilation and increased blood flow.
- PDE1C/cAMP/PKA Cascade: The research points to a specific signaling pathway where the transcription factor NKX2-3 influences the activity of PDE1C. This, in turn, results in a decrease in cyclic AMP levels and reduced activation of PKA, culminating in diminished calcium channel activity and pericyte relaxation.
These observations reveal a tangled interplay between pericyte behavior and vascular function. On a broader scale, they show that subtle changes at the cellular level can have dramatic effects on the overall tumor environment, making the path to metastasis both delicate and highly orchestrated.
How Tumor Cells Exploit These Vascular Dynamics
When we take a closer look at the forces that facilitate metastasis, it becomes evident that tumor cells are highly adept at exploiting the local vascular environment. The nerve-racking process of tumor cell intravasation—the step in which cancer cells penetrate blood vessel walls—is not merely a random accident. Instead, it is greatly assisted by tumor pericyte behavior.
In the metastatic cascade, the following steps are critical:
- Intravasation: This refers to the entry of tumor cells into the bloodstream. A relaxed vascular system, characterized by increased vessel diameter and leakiness, offers the perfect passageway for tumor cells.
- Circulation: Once in the bloodstream, the tumor cells must survive the turbulent journey. The local hemodynamics, including blood flow speed and shear stress, critically impact their survival.
- Extravasation: Finally, escaping the bloodstream and colonizing distant organs requires that tumor cells latch onto and traverse the vessel wall—another step potentially eased by enhanced vessel permeability.
The research underscores that the subtle parts of the tumor vascular microenvironment—the little details of how pericytes manage blood flow—play a pivotal role in each transition of the metastatic process. Understanding these interactions may enable clinicians to better predict metastasis risk and develop therapies that can “lock down” the blood vessels, thereby preventing escape routes for the tumor cells.
Unraveling the Hidden Mechanisms: The NKX2-3 Factor and its Downstream Effects
A standout finding in this study is the identification of the transcription factor NKX2-3 as a key regulator in tumor pericytes. The research shows that increased expression of NKX2-3 in pericytes is associated with enhanced vessel dilation and vascular leakiness. The calm unraveling of the molecular chains behind this process involves several intricate steps:
- Upregulation of NKX2-3: Elevated levels of NKX2-3 were observed particularly in pericytes derived from tumors with liver metastasis. The study suggests that this upregulation is triggered by tumor-derived extracellular vesicles (EVs).
- Role of LncRNA NEAT1: The tumor cells release EVs rich in the long noncoding RNA NEAT1, which then enters the pericytes. Once inside, NEAT1 sponges (or binds) to microRNA-769-5p, reducing its capacity to suppress NKX2-3 expression. In practical terms, this means that the release of NEAT1-packed EVs creates a cascade effect leading to amplified NKX2-3 levels.
- PDE1C/cAMP/PKA Pathway: NKX2-3 then modulates the pericyte contraction process by suppressing calcium influx through the PDE1C/cAMP/PKA signaling axis. Essentially, when NKX2-3 is high, there is less calcium available to drive pericyte contraction, and as a result, the pericytes remain relaxed.
This series of events turns a normally controlled cellular process into a scenario that favors metastasis—a clear example of how hidden complexities in tumor biology can have large-scale consequences. The study’s detailed analysis of the nitty-gritty reveals the fine shades and little twists involved in pericyte signaling, providing a new framework for understanding therapy resistance and cancer spread.
Potential Therapeutic Strategies: Targeting Pericyte Function and Vascular Dynamics
Given the super important role that NKX2-3 high pericytes seem to play in facilitating metastasis, researchers are now exploring ways to counteract these effects. One promising approach is to block the transcriptional activity of NKX2-3, thereby restoring normal pericyte contraction and reducing the undesired vessel dilation that aids tumor cell dissemination.
Peptide-Based Inhibitors
One outstanding strategy highlighted in the study involves the development of synthetic peptides capable of interfering with NKX2-3’s function. These oligopeptides are engineered to bind with high affinity to key downstream targets, such as the PDE1C promoter—a move aimed at halting the cascade that leads to pericyte relaxation. The process involves several key points:
- Design and Synthesis: Using advanced prediction tools like AlphaFold, researchers identified the fine details of NKX2-3’s structure. With this information, several candidate oligopeptides were synthesized.
- Targeting Efficiency: Among the candidates, one peptide (referred to as NB2) showed exceptional promise in its ability to block the binding between NKX2-3 and the PDE1C promoter.
- Tumor-Specific Delivery: To ensure the peptides act primarily on tumor pericytes rather than all pericytes in the body, the peptides were coupled with a prodrug that is activated by fibroblast activation protein α (FAPα). This enzyme is often present in higher levels in tumor pericytes, making it an ideal marker for targeted delivery.
By incorporating this targeted peptide strategy, the researchers successfully induced vasoconstriction in the tumor environment in experimental models. The effect was clear: reduced blood flow, enhanced vessel integrity, and—most importantly—a significant drop in metastatic spread. These findings open the door for custom therapies that hone in on the small distinctions between normal and tumor-associated vascular cells.
Other Prospective Approaches
Beyond peptide-based inhibitors, there are several alternative avenues that merit further investigation:
| Strategy | Description | Potential Benefits |
|---|---|---|
| Monoclonal Antibodies | Targeting surface markers uniquely overexpressed on tumor-associated pericytes. | High specificity with potential for combination with existing immunotherapies. |
| RNA Interference | Using siRNA or shRNA to reduce the levels of NKX2-3 or related transcripts in pericytes. | Directly reduces the gene expression responsible for tumor vessel relaxation. |
| Small Molecule Inhibitors | Design compounds that disrupt key protein-protein interactions in the PDE1C/cAMP/PKA pathway. | May offer oral bioavailability and easier administration compared to peptide drugs. |
Each of these strategies presents its own set of challenges and benefits. The complex interplay between tumor cells and their surrounding niche means that any effective therapy must be precisely calibrated, ensuring that normal vascular functions are maintained while the metastasis-promoting mechanisms are selectively blocked.
Clinical Implications: Managing the Tumor Microenvironment to Fight Metastasis
The clinical ramifications of this research are immense, particularly when it comes to designing new treatments that address the nerve-racking process of cancer metastasis. The present findings provide a fresh perspective on how the local vascular environment can be manipulated to block the escape routes of tumor cells.
Diagnostics and Predictive Biomarkers
One immediate implication of the study is the potential for developing diagnostic markers that evaluate the state of the tumor vasculature. For instance:
- Vessel Diameter and Blood Flow Measurement: Advanced imaging techniques, such as computed tomography and ultrasound Doppler imaging, can assess vessel dilation in tumors. Increased blood flux and wider vessel diameters may serve as predictive markers for metastasis.
- Molecular Markers: Elevated levels of NKX2-3 or decreased calcium channel activity in pericytes could be indicative of a tumor’s metastatic potential. Potential blood tests might measure circulating biomarkers related to these pathways.
Early and precise diagnosis may allow clinicians to tailor treatments more specifically to patients at high risk for metastasis, thereby increasing the chances of successful intervention before the cancer spreads beyond the primary site.
Integrating New Therapies with Existing Treatments
Given that metastasis is the primary cause of cancer death, any new treatments that can limit cancer spread are extremely valuable. Combining new pericyte-targeting agents with conventional chemotherapy, radiation therapy, or immunotherapy might provide a multi-pronged approach to cancer treatment. For example:
- Combination Regimens: A therapy that induces vasoconstriction may be used in tandem with cytotoxic agents. By locking down the vascular system, these drugs may prevent tumor cells from dispersing, thereby giving traditional therapies a better chance to eliminate the primary tumor.
- Sequential Treatment Plans: It may also prove beneficial to treat patients first with pericyte-targeting inhibitors to stabilize the vascular network before proceeding with other treatments that directly target tumor cells.
This kind of integrated approach promises to tackle metastatic cancer at more than one level, reducing the chances for cancer cells to escape and survive in distant organs.
Looking Ahead: Challenges and Future Directions
Despite these promising insights, several confusing bits and challenging issues remain. The tumor microenvironment is a tangled mix of cells, signals, and structures that continuously change over time. Some of the key off-putting challenges include:
- Selective Targeting: Ensuring that therapies aimed at pericytes do not interfere with normal vascular functions in healthy tissues is a major concern. Pericytes are vital for normal blood vessel maintenance, and widespread interference could lead to undesirable side effects.
- Disease Heterogeneity: Tumors can vary significantly between patients and even within the same tumor. The varied expression of NKX2-3 and associated molecules calls for personalized treatment regimens.
- Long-Term Efficacy: While initial results are encouraging, it remains to be seen whether these strategies can produce long-lasting benefits in patients. The potential for tumors to adapt and find alternative routes for metastasis means that any single approach may have limited durability on its own.
These challenges, although intimidating, are not insurmountable. Each issue provides a window into further research questions that might lead to even more effective cancer therapies. As we take a closer look at the hidden complexities of the tumor microenvironment, it becomes clear that a comprehensive strategy combining diagnostics, targeted therapy, and conventional treatments could be key to managing metastatic disease.
Insights into the Tumor Microenvironment: Reflections on the Study’s Broader Context
For too long, the process of metastasis was primarily viewed through the lens of tumor cell mutations and their migratory abilities. This study shifts the focus to the supportive role of the surrounding environment, particularly the blood vessels and the pericytes that regulate them.
It is increasingly apparent that understanding the little twists of the tumor microenvironment involves not just studying the tumor cells themselves but also appreciating the interplay of various supporting cells and signals. Key takeaways include:
- Intercellular Communication: Tumor-derived extracellular vesicles are central messengers that alter the behavior of pericytes. By delivering molecules such as lncRNA NEAT1, these vesicles modulate gene expression in recipient cells, thereby influencing vascular dynamics.
- Fine Points of Signaling Pathways: The PDE1C/cAMP/PKA pathway is a prime example of a cascade where slight changes can translate into major structural and functional differences at the tissue level. Understanding these fine shades could help identify additional targets for therapy.
- Balancing Act: There is a need to find the right balance between inhibiting the metastatic process and maintaining the integrity of normal vascular function. This delicate balance epitomizes many of the subtle distinctions in modern cancer therapy.
These insights encourage us to take a broader view of metastasis as not merely a problem of unstable tumor cells but as a multifaceted issue involving the support network that tumors build for themselves. By appreciating and addressing these interconnected issues, the medical community may find new avenues for intervention that were previously overlooked.
Making Your Way Through Cancer’s Twists and Turns: Final Thoughts
The findings discussed in this editorial underscore how the local vascular environment, shaped by tumor pericytes and their signaling pathways, is super important in the process of metastasis. In particular, the role of NKX2-3 in modulating pericyte behavior offers a promising target for novel therapeutic strategies. By effectively “locking down” the tumor blood vessels, we may be able to cut off a crucial escape route that cancer cells exploit.
For clinicians and researchers alike, these discoveries are both encouraging and a reminder of how much remains to be understood about the tumor microenvironment. The study demonstrates that the seemingly minute details of pericyte function and intracellular signaling can have sweeping consequences in the broader narrative of cancer progression.
In addition, the study highlights the importance of looking at cancer as a systemic disease. Metastasis is not just about the tumor cells breaking free from their original site; it is equally about how they interact with and manipulate their surrounding environment—the very blood vessels that normally serve vital physiological roles.
Looking forward, further studies will need to focus on several key areas:
- Refining Diagnostic Tools: Advances in imaging and molecular profiling are necessary to better assess the state of the tumor vasculature in individual patients. This will allow for more precise risk assessment and tailored treatment strategies.
- Optimizing Targeted Therapies: Peptide-based inhibitors and other targeted treatments must be carefully developed to maximize efficacy while minimizing side effects. Ongoing clinical trials will be essential to validate these promising approaches in a real-world setting.
- Investigating Combined Modalities: Integrating pericyte-targeting agents with existing treatments—including chemotherapy, radiation, and emerging immunotherapies—could offer a more comprehensive approach to stopping metastasis. It is essential to work through the best methods for combining these modalities to achieve the best patient outcomes.
Ultimately, the research reviewed here represents an important step forward in our understanding of metastasis. It reminds us that the journey of a cancer cell from a primary tumor to a distant organ is guided by many subtle details, from the molecular signals inside pericytes to the overall architecture of the tumor vasculature. By addressing these complicated pieces, we can start to figure a path toward more effective therapies that not only target tumor cells directly but also the supportive environment that allows them to thrive and spread.
This study also sets the stage for a broader discussion on how rethinking the role of the tumor microenvironment may lead to significant breakthroughs in cancer treatment. It is a call to action for medical scientists and practitioners to pay close attention to the hidden complexities that lie beneath the surface of what we once thought of as a simple transactional process of cell migration and colonization.
There is a clear need to dig into these challenging aspects of cancer biology further. The twists and turns of tumor vasculature regulation are not just academic interests—they have real, tangible consequences for how we diagnose, treat, and ultimately manage cancer. As we figure out the subtle details of how pericytes and other components shape the metastatic landscape, we move one step closer to transforming metastatic cancer from a devastating disease to one that can be effectively controlled.
Conclusion: Charting a New Course in Metastatic Cancer Management
In summary, the compelling research on tumor pericytes reveals that the regulation of local vascular tone and hemodynamics is a critical factor in cancer metastasis. The interplay between NKX2-3, the PDE1C/cAMP/PKA signaling cascade, and extracellular vesicle-mediated regulation illustrates the many small distinctions that can cumulatively have a huge impact on the course of the disease.
By integrating innovative therapeutic strategies, such as targeted peptide prodrugs, with traditional treatment methods, we have an opportunity to change the way metastatic cancer is managed. Recognizing and working through the tangled issues, confusing bits, and intricate pathways in pericyte signaling, researchers and clinicians can collaborate to develop treatments that not only combat the primary tumor but also prevent its spread.
As we take a closer look at the inner workings of the tumor microenvironment, it becomes increasingly clear that every detail matters. The success of future cancer therapies will rely on our ability to figure a path through these challenging, often off-putting, yet ultimately crucial facets of cancer biology. The road ahead is filled with obstacles, but with careful study and targeted strategies, we have a strong chance of curbing metastasis and saving lives.
In this era of rapid advancements in precision medicine and personalized treatments, the insights gleaned from the study of tumor pericytes offer a promising beacon. By addressing the nerve-racking challenges, making your way through the twists and turns of cellular signaling, and embracing the key details of the tumor microenvironment, we pave the way for a future where metastatic cancer is not only treatable but potentially preventable.
Ultimately, this new perspective on the role of pericytes in cancer metastasis invites us to reimagine our strategies and refine our approach to cancer treatment. When the finer points of vascular dynamics are fully understood and effectively manipulated, the prospect of stopping metastasis before it even starts becomes a real possibility—a possibility that holds immense promise for patients and clinicians alike.
Originally Post From https://www.nature.com/articles/s41467-025-62475-6
Read more about this topic at
Pericytes promote metastasis by regulating tumor local …
Pericytes limit tumor cell metastasis – PMC

